Abstract
PURPOSE: This narrative review of research conducted during the first 2 years of the COVID-19 pandemic examines whether alcohol use among cisgender women and transgender and nonbinary people increased during the pandemic. The overarching goal of the review is to inform intervention and prevention efforts to halt the narrowing of gender-related differences in alcohol use.
SEARCH METHODS: Eight databases (PubMed, APA PsycInfo, CINAHL, Embase, Scopus, Gender Studies Database, GenderWatch, and Web of Science) were searched for peer-reviewed literature, published between March 2020 and July 2022, that reported gender differences or findings specific to women, transgender or nonbinary people, and alcohol use during the pandemic. The search focused on studies conducted in the United States and excluded qualitative research.
SEARCH RESULTS: A total 4,132 records were identified, including 400 duplicates. Of the remaining 3,732 unique records for consideration in the review, 51 were ultimately included. Overall, most studies found increases in alcohol use as well as gender differences in alcohol use, with cisgender women experiencing the most serious consequences. The findings for transgender and nonbinary people were equivocal due to the dearth of research and because many studies aggregated across gender.
DISCUSSION AND CONCLUSIONS: Alcohol use by cisgender women seems to have increased during the pandemic; however, sizable limitations need to be considered, particularly the low number of studies on alcohol use during the pandemic that analyzed gender differences. This is of concern as gender differences in alcohol use had been narrowing before the pandemic; and this review suggests the gap has narrowed even further. Cisgender women and transgender and nonbinary people have experienced sizable stressors during the pandemic; thus, understanding the health and health behavior impacts of these stressors is critical to preventing the worsening of problematic alcohol use.
Introduction
Although historically cisgender women (i.e., women whose sex assigned at birth is consonant with their gender) in the United States have had lower levels of alcohol consumption than cisgender men, recent analyses of historical and cohort data suggest that overall gender differences are narrowing.1 This narrowing is largely due to substantial increases in cisgender women's alcohol use, binge drinking (operationalized as four or more drinks in 1 day for cisgender women; five or more drinks in 1 day for cisgender men)1,2 and alcohol use disorder (AUD; meets criteria for past 12-month dependence or abuse as established in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders [DSM-V]).3 Cisgender women also report more barriers to treatment4,5 and lower treatment utilization than cisgender men.6-9 Given that cisgender women may experience more severe alcohol-related problems (e.g., problems in relationships or at work10) and health impacts than do cisgender men, even at lower levels of alcohol use,11 understanding whether the pandemic has led to an increase in alcohol use among cisgender women is critically important.
Rates and risks for problematic alcohol use vary by sexual identity,12-14 race/ethnicity,15 and other factors, including socioeconomic status and relationship status.16 These differences may be partially explained by differences in stress levels, including economic stressors and psychological distress17 and may have been further modified by the coronavirus disease 2019 (COVID-19) pandemic. Research on mental health during the pandemic suggests that cisgender women experienced elevated rates of stress, anxiety, and depression compared to pre-pandemic rates,18-20 at least in the early stages of the pandemic. In contrast, some research has suggested no gender differences in pandemic-related emotional distress.21,22
Stress is one of the strongest predictors of substance use, including alcohol use,23 and higher levels of stressors increase risks for problematic alcohol use, including AUD.24,25 The COVID-19 pandemic often has been described as a "perfect storm" of multiple sources of stress and has been linked to worsened mental health and health behaviors overall.21,22,26-29 There is evidence of increased problematic alcohol use during previous pandemics;30 however, the COVID-19 pandemic is unique among recent pandemics in the breadth and duration of its impacts and thus may have more substantial effects on health and well-being, including alcohol use. Cisgender women, compared to cisgender men, may be particularly affected by the pandemic due to higher levels of stressors.31,32 These stressors may be related to negotiating working from home28 while balancing remote schooling for children,21,28 higher likelihood of working in frontline and/or caregiver jobs,28,33 increased risks for intimate partner violence,34-38 delays in accessing needed health care,39 isolation,40-42 and potentially higher risks for unintended pregnancies.31 In a prospective study of families, cisgender women, compared to cisgender men, reported higher levels of stressors across four out of five domains. Specifically, cisgender women experienced higher levels of stressors in work/finances (31% increase), home disruptions (64%), social isolation (13%), and health care barriers (94%).42 The burden of pandemic-related stressors, combined with chronic and cumulative stressors disproportionately impacting cisgender women (e.g., sexism and/or violence across the life span43), may result in allostatic overload, which heightens health risks.44 When faced with higher levels of stressors during the pandemic, cisgender women may be at higher risk than cisgender men for alcohol consumption because cisgender women are more likely than cisgender men to use alcohol to cope with negative emotions.24,45 Using alcohol to cope may have potentially disproportionate impacts on those experiencing the highest levels of stressors (e.g., frontline workers, parents).42
Transgender and nonbinary (TNB, i.e., people whose gender differs from their sex assigned at birth) individuals experience significant health disparities, and their health is negatively affected by high levels of stigma, discrimination, and violence, as well as low levels of support.46-51 The COVID-19 pandemic may have been particularly stressful for TNB people compared to cisgender people due to elevated socioeconomic impacts such as job loss,52 food52 and housing insecurity,53,54 as well as reductions in social and community support.55-57 TNB people also have experienced disruptions to medical care (including gender-affirming services), which heightens stress.53,56 Coping is a key motivation for alcohol use among TNB populations,51,58,59 which might suggest increased use of alcohol to cope during a stressful event such as a global pandemic. Yet, research findings on rates of alcohol use among TNB populations are more mixed compared to cisgender people.60-64 Problematic alcohol use is associated with increased risks for secondary harms that disproportionately affect TNB individuals, such as suicidal ideation, intimate partner violence, sexual violence, and the exacerbation of mental and physical health problems,62,65,66 highlighting the importance of a deeper understanding of alcohol use among TNB individuals. Additionally, TNB people experience barriers to treatment,67 including a lack of culturally responsive care options68-73 and discrimination by providers.68 Of note, the umbrella term "TNB" encompasses a diverse range of identities and experiences, but existing research often does not disentangle this diversity, instead aggregating across groups who fall outside of cis-normative gendered expectations and who then are compared with cisgender peers.
Understanding alcohol use among cisgender women and TNB people during the pandemic is particularly important due to risks for severe health outcomes. Not only are COVID-19 patients with AUD more likely to be hospitalized and to have higher all-cause mortality,74 but alcohol-related mortality spiked with the onset of the COVID-19 pandemic.75,76 Problematic alcohol use also is a major risk factor for COVID-19 infections and mortality.77 Although the connections between COVID-19 and alcohol use have widespread effects, specific alcohol-related health impacts of the pandemic have been particularly harmful for cisgender women, as indicated by a 125% increase in alcohol-associated hepatitis78 and a stark increase in the proportion of patients screening positive for substance use (including alcohol use) in emergency departments.79 To our knowledge, similar research has not been done among TNB populations.
This review aims to understand the unique experiences of cisgender women and TNB people, as well as among understudied groups of cisgender women such as women of color, sexual minority women (SMW, e.g., lesbian, bisexual, queer women), and older women to describe subgroup impacts of the COVID-19 pandemic on alcohol use. A recent scoping review of substance use during the pandemic noted the importance of examining substance use (including alcohol) during the pandemic among cisgender women and TNB populations.80 Thus, this review aims to evaluate the extant literature testing whether cisgender women drank at similar or higher levels than cisgender men during the pandemic. The review further explores alcohol use among TNB populations during the pandemic, with a focus on gender differences in rates of alcohol use (e.g., binge drinking, alcohol dependence, quantity/frequency of drinking) in research conducted during the pandemic (since March 2020) in the United States.
Methods
Search Methods Employed
This narrative review of alcohol use during the pandemic was conducted to document whether alcohol use had increased among women—a population already experiencing inclines in alcohol use before the pandemic—and among TNB people in order to inform needed prevention and interventions, as well as to inform policy. The review process included seven steps:81-83 (1) refining the topic and identifying the research question; (2) developing a protocol; (3) identifying relevant studies; (4) screening and selecting studies; (5) extracting the data; (6) critically appraising and synthesizing the data; and (7) reporting the results.
One author, a Health Sciences Library Informationist conducted the literature searches on July 15, 2022, in eight databases: PubMed (pubmed.gov); APA PsycInfo (EBSCO); CINAHL [Cumulative Index to Nursing and Allied Health Literature] (EBSCO); Embase (embase.com); Scopus (scopus.com); Gender Studies Database (EBSCO); GenderWatch (ProQuest); and Web of Science (webofscience.com). Because the review addresses two separate questions, two search strategies were used. The first strategy comprised a combination of search strings related to alcohol use, COVID-19, and women. The second strategy combined search strings for alcohol use, COVID-19, SMW, and TNB populations. No filters were applied to the search results.
All records found via the database searches were exported to an EndNote library (version X9). Duplicates were identified and removed in EndNote, and the remaining library was imported into the Covidence review software to facilitate identifying relevant articles for the narrative review. Articles were eligible for inclusion in this review if they met the following criteria hierarchically: (1) were published in peer-reviewed journals between March 2020 and July 2022; (2) were written in English; (3) used human participants in the United States (to reduce variability in responses to the pandemic); (4) included measurement of alcohol use (broadly defined); (5) collected data during the COVID-19 pandemic; and (6) included analyses of gender differences in rates of alcohol use or focused solely on cisgender women or TNB people and alcohol use during the pandemic. Articles were excluded if they were review papers or qualitative studies, if they did not conduct any gender differences analyses (unless the study focused on women or TNB samples only), and if alcohol was not an outcome.
Data Extraction
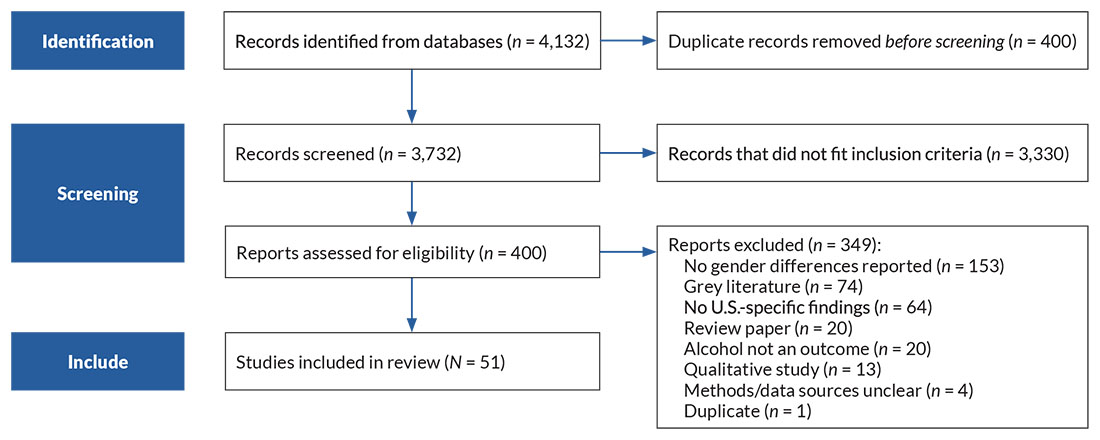
After conducting a title and abstract review of all articles, the authors reviewed the full text of the remaining papers to determine final inclusion. Differences were discussed amongst three authors until agreement was reached. The full texts of the 400 articles were assessed for relevance to the review's aims. When an article was excluded during the full review, authors documented the reason for its exclusion. (See Figure 1 for the search strategies for both questions combined.) Three authors critically reviewed and synthesized data from the 51 included articles.
Figure 1. PRISMA flow diagram of search strategy used during the narrative review of women's alcohol use during the pandemic. Note: PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Results
Results of the Literature Search
The literature search identified a total of 4,132 records. There were 400 duplicates, leaving 3,732 unique records for consideration in the review; of these, 51 articles ultimately were included.
Results of the Reviewed Studies
Appendices 1 and 2 (located after the references) list the 51 reviewed articles and include all data from the abstraction protocol. Consistent with the goals of a narrative review, potential methodological limitations of the research are highlighted to help the reader better evaluate the validity and generalizability of the findings. The results are broken into four sections: (1) prevalence; (2) specific populations and demographic differences (age, race/ethnicity) or life experiences (pregnancy, intimate relationships, frontline work); (3) linkages between alcohol and mental health, stress, or coping; and (4) TNB individuals and SMW.
Table 1 includes descriptive data of the studies reviewed. Of those, 24% included nationally representative samples, 36% included pre-pandemic data (as opposed to retrospective reporting or only having within-pandemic data), 51% had data collection that ended early in the pandemic (March–May 2020), and 16% had data collection that ended in 2021. Slightly more than one-quarter (26%) used the Alcohol Use Disorders Identification Test (AUDIT) or AUDIT-Consumption (AUDIT-C), with several studies using just one or two items from the AUDIT. In addition, 6% used another validated measure, and 29% examined quantity and frequency only. Of those studies that looked at gender differences (as opposed to having a sample of cisgender women only), 73% found gender differences in alcohol use.
Table 1. Descriptives of Studies Included in Review| | | n | % |
|---|
| Data collection start | Early pandemic (March–May 2020) | 26 | 51.0% |
| Late 2020 | 7 | 13.7% |
| Pre-pandemic | 18 | 35.3% |
| Data collection end | Early pandemic | 26 | 51.0% |
| Late 2020 | 17 | 33.3% |
| Early 2021 | 7 | 13.7% |
| Late 2021 | 1 | 2.0% |
| Study design | Prospective | 20 | 39.2% |
| More than one cross-sectional time point | 7 | 13.7% |
| Cross-sectional | 24 | 47.1% |
| Samples included | Cisgender women only | 4 | 7.8% |
| Cisgender women and men | 33 | 64.7% |
| Cisgender women, men, and TNB people | 4 | 7.8% |
| Cisgender women and TNB people | 10 | 19.6% |
| Comparison groups | Cisgender men | 36 | 70.6% |
| TNB individuals | 1 | 2.0% |
| Cisgender men and TNB individuals | 9 | 17.6% |
| No comparison group | 5 | 9.8% |
| Sample recruitment | Nationally representative | 12 | 23.5% |
| Convenience | 8 | 15.7% |
| Convenience: Online/social media | 20 | 39.2% |
| Clinic sample | 5 | 9.8% |
| Undergraduates (various recruitment methods) | 5 | 9.8% |
| Other | 1 | 2.0% |
| Drinking measurement | AUDIT or AUDIT-C | 13 | 25.5% |
| Daily drinking questionnaire | 3 | 5.9% |
| Quantity and frequency | 15 | 29.4% |
| Quantity | 3 | 5.9% |
| Frequency | 7 | 13.7% |
| Perceptions | 5 | 9.8% |
| Other validated scale | 3 | 5.9% |
| Other | 2 | 3.9% |
| How change was measured | Pre- and post/during pandemic data | 10 | 19.6% |
| Retrospective recall of pre-pandemic AUDIT | 1 | 2.0% |
| Retrospective report of current drinking in past vs drinking now | 4 | 7.8% |
| Self-perceived changes in alcohol use | 14 | 27.5% |
| Self-report of current drinking at more than one time point | 12 | 23.5% |
| Did not measure changes in drinking | 10 | 19.6% |
Note: AUDIT, Alcohol Use Disorders Identification Test; AUDIT-C, AUDIT-Consumption; TNB, transgender or nonbinary
Table 2. Summary of Results for Changes in Drinking After Onset of COVID-19 Pandemic| | Number of Possible Studies | Proportion With Finding* |
|---|
| n | % |
|---|
| Overall | Alcohol use or problems increased | 20 | 12 | 60.0% |
| Alcohol use or problems decreased | 20 | 5 | 25.0% |
| Alcohol use or problems did not change | 20 | 3 | 15.0% |
| Cisgender Women | Alcohol use or problems increased | 13 | 8 | 61.5% |
| Alcohol use or problems decreased | 13 | 2 | 15.4% |
| Alcohol use or problems did not change | 13 | 3 | 23.1% |
| Cisgender Men | Alcohol use or problems increased | 13 | 6 | 46.2% |
| Alcohol use or problems decreased | 13 | 3 | 23.1% |
| Alcohol use or problems did not change | 13 | 4 | 30.8% |
| Transgender and Nonbinary Individuals | Alcohol use or problems increased | 1 | 1 | 100% |
| Alcohol use or problems decreased | 1 | 0 | 0% |
| Alcohol use or problems did not change | 1 | 0 | 0% |
*Percentages within each group may not total 100% due to rounding. Note: COVID-19, coronavirus 2019.
Of the 51 studies that met inclusion criteria, 20 studies tested for trends over time in alcohol use, including the pandemic period. Table 2 summarizes the results of those 20 studies, including the number of studies that found increases, decreases, or no change in alcohol use. Overall, 12 of the 20 studies documented increases in alcohol use during the pandemic period. More studies documented increases among cisgender women than among cisgender men (8 and 6 out of 13, respectively), and the only study with sufficient data to test for trends among TNB individuals found increases in alcohol consumption.
The following sections present the results in more detail, organized by prevalence data; specific subpopulations; stress, coping, and mental health; and alcohol use among SMW and TNB people. Not all studies had mutually exclusive samples; thus, studies may be mentioned in more than one section.
Prevalence
Eighteen studies were primarily aimed at describing prevalence of alcohol use among adults during the pandemic and included analyses of gender differences. These studies were divided into two groups: cross-sectional studies (including repeated cross-sectional studies) of adults and longitudinal/prospective studies of adults.
Cross-sectional general population adult studies
Nine cross-sectional studies,79,84-91 all conducted during the early pandemic, met inclusion criteria. All used convenience samples, with two samples recruited from social media. In three studies that asked participants to compare retrospectively their pre-pandemic AUD symptoms to current symptoms,85-87 all found increased reports of AUD symptoms among cisgender women during the early pandemic compared with retrospective reports of pre-pandemic symptoms. In one study, cisgender men also reported increases;85 in another, they did not;86 and in the third study cisgender women reported increased drinking more often than did cisgender men.87 A fourth study found no gender differences in self-defined "drinking behaviors" during the early pandemic.88 Across these studies, the cross-sectional design—including retrospective reporting of pre-pandemic drinking behaviors and AUD symptoms as well as use of convenience samples based on volunteers from social media—limit the conclusions that can be drawn from these studies.
Three general population adult studies used repeated cross-sectional assessments (with different samples at each time point) before and during the pandemic to compare rates across time.79,84,89 Using nationally representative samples, Kerr et al.89 documented that daily drinking and alcohol volume were higher among cisgender women interviewed during the pandemic through 2021 compared to those interviewed pre-pandemic. AUD prevalence across the continuum from mild to severe was also higher during the pandemic. Sensitivity analyses indicated that results were robust to the timing of interviews and thus unlikely to be affected by pandemic-related social distancing policies. Electronic health record data of more than 100,000 patients visiting emergency departments showed higher alcohol admissions and evaluations for cisgender women during the pandemic compared with rates before the pandemic.79 In contrast, expenditure data, as an indirect measure of alcohol consumption, indicated lower household alcohol expenses during the pandemic, compared with pre-pandemic levels, for both cisgender men and cisgender women. However, expenditures may not correlate precisely with volume sales—for example, if purchases moved from on-premise to off-premise.84
Repeated cross-sections of data provide sufficient rigor for assessing changes in time trends, and all three studies included pre-pandemic time points, a notable strength. Given that two of the three studies found that increases in relatively serious alcohol-related harm (e.g., AUD, alcohol-related emergency department admissions) are concentrated among cisgender women, these data indicate an emerging concern.
Longitudinal general population adult studies
Nine longitudinal studies of adults in the general population met inclusion criteria.92-100 Three of these were based on a single data source, the Understanding America Study (UAS),92,95,97 a nationally representative panel study conducted monthly, with published data through mid-2020. All three studies from UAS demonstrated increases in alcohol consumption during the pandemic using repeated-measures longitudinal analyses, including increases in drinking days and near-daily drinking among cisgender women. However, these increases generally were less than those seen in cisgender men and remained below drinking levels among cisgender men.92,95,97 In a representative online sample of adults, among those who reported any alcohol use, cisgender men had higher levels of alcohol use (i.e., average number of drinks per day) than cisgender women at baseline (April–June 2019). However, alcohol use in cisgender men declined over time (last wave of data collection was in March 2021), whereas it stayed the same over time in cisgender women.100 In an additional nationally representative study with data from 2019 through the early months of the pandemic, days consuming alcohol and heavy drinking days (defined as five or more drinks within "a couple of hours" for cisgender men and four or more drinks for cisgender women) increased among cisgender women.99 Of note, however, no longitudinal studies of the general adult population included data beyond January 2021, and no studies published in 2022 met inclusion criteria for this review.
Given that surveys were completed by telephone both before and during the pandemic, it is unlikely that study methodology was substantially impacted by COVID-era research policies, although an impact on willingness to participate in research (either more or less willing) cannot be excluded and could be a limitation. However, taken together, the available research indicates that days consuming alcohol and heavy drinking days on average increased among cisgender women in the general population during the early and middle periods of the pandemic, but that for both variables, their consumption levels largely remained lower than, and did not change at the same rate as, those of cisgender men.
Specific Populations and Demographic Differences
Several studies focused on unique subpopulations of cisgender women and alcohol use during the pandemic. The following sections discuss unique impacts on different age groups, different racial/ethnic populations, cisgender women in couple relationships, those who are pregnant or who are parents, and those who are frontline workers.
Adolescents, young adults, and older adults
Five cross-sectional studies met inclusion criteria; four101-104 were among young adult college undergraduates, and one was a nationally representative survey of high school students.105 No study had pre-pandemic data, and data collection spanned from early in the pandemic through early 2021. In the only nationally representative study of high school students meeting inclusion criteria,105 cisgender women students had higher rates of current alcohol consumption (defined as at least one drink in the past 30 days) than cisgender men students but did not report that they thought they drank more due to the pandemic. A cross-sectional survey of undergraduate college students conducted in fall 2020, with retrospectively reported pre-pandemic drinking, indicated increased consumption during the pandemic among all groups.103 Moreover, consumption and increases in consumption were greater among cisgender men compared with cisgender women and TNB individuals. Sexual minority groups generally reported higher levels of alcohol consumption and greater increases compared with pre-pandemic levels in both the high school and college samples; however, none of the studies examined interactions between sexual identity and gender. When coupled with the use of convenience samples, the cross-sectional designs and retrospective reporting limit inference from studies among college students.
Two studies included repeated cross-sectional samples of college students,103,104 one of which included pre-pandemic data collection.103 AUD prevalence was higher during the pandemic compared with pre-pandemic, with increases concentrated among cisgender women compared with cisgender men. For example, 49.7% of cisgender women met criteria for AUD during the pandemic, compared with 34.4% before the pandemic.
Seven studies106-112 included longitudinal data among young adults (two of the seven from the same data source109,110). All had pre-pandemic data points, a major strength of the evidence base. However, the span of pandemic data collection was limited to the early pandemic through late 2020. Two had nationally representative data (most used convenience samples).108,112 Most of these studies only reported data through spring 2020, which provides a limited assessment of pandemic-era changes in alcohol consumption, and findings regarding gender differences were mixed. Five of seven studies reported no gender differences in drinking as indicated by average past 3-month drinking quantity;108 self-assessment of changes in drinking during the pandemic; and binge drinking (i.e., five or more drinks in a row).110,111 A sixth study reported higher odds of drinking (any drinking on previous day) among cisgender men compared with cisgender women but noted no changes during the pandemic period.112
The remaining studies of college students and young adults generally found either faster declines in drinking among cisgender men,106 or faster increases,109 compared with cisgender women. A study comparing alcohol consumption during college spring semester across 3 years (2018, 2019, and 2020) found that whereas alcohol consumption (operationalized as number of drinking days and drinks per day) generally increased during spring semesters pre-pandemic, alcohol consumption either did not increase or declined in 2020 depending on the measure;107 no gender differences were found. The most robust studies (e.g., Jaffe et al. 2021107) indicate that college drinking largely declined in the early pandemic period, which is expected as students moved off campus, but there is little evidence for gender differences in these declines.
In sum, research among college students and young adults is mixed. Some studies found higher levels of alcohol use among cisgender men and some among cisgender women; however, overall, there were no increases in alcohol use among cisgender young women during the pandemic. Only one study identified for this review focused on older adults.113 In this study, which included a nationwide sample of older adults, cisgender women accounted for 59% of those who reported drinking more than usual during the pandemic.
Demographic differences by race/ethnicity
Only two studies focused on race/ethnicity and alcohol consumption during the pandemic.114,115 Among a sample of American Indian cisgender women followed prospectively through October 2021, approximately a quarter reported self-perceived increased consumption and half reported binge drinking (i.e., four or more "standard" drinks per day) during the pandemic.114 Among Black, indigenous, and other people of color (BIPOC) undergraduate students prospectively followed from before the pandemic through spring 2020, declines in drinking frequency were reported, but cisgender women, compared with cisgender men, were less likely to show declines.115 Overall, the sparse research is mixed on alcohol use among BIPOC cisgender women during the pandemic, suggesting that more research is needed.
Couple relationships and pregnancy
Three studies that met criteria for inclusion examined potential differences in alcohol use among cisgender women and their partners in heterosexual couple relationships and among cisgender pregnant women; one study also investigated how early parenthood might impact cisgender women's alcohol use during the pandemic.116-118 The study of cisgender women and their men partners during the pandemic detected no gender differences in drinking levels; however, cisgender men reported more alcohol problems than did cisgender women. Cisgender women's general stress and financial stress had no impacts on their partners' drinking (drinks per week); however, cisgender men's stress was associated with an increase in their partners' drinking and a 22% increase in their own and their partners' high-intensity drinking (defined as 10 or more drinks per day for men and eight or more drinks per day for women).118
There are mixed findings among pregnant cisgender women in reports of changes in alcohol use during the pandemic. Among a convenience sample of pregnant cisgender women, 11% reported perceived increases in their own and 28% in their partners' alcohol use since the pandemic's beginning. In contrast to these findings, none of the pregnant cisgender women in a study of centers for high-risk pregnancies reported self-perceived increases in alcohol use since the start of the pandemic.116 Notably, in the same study, 10% of postpartum cisgender women reported increased alcohol use.116
Together these findings suggest that in couple relationships during the pandemic, cisgender men's stress levels and drinking may be associated with increased alcohol use and high intensity drinking among cisgender women. Findings among pregnant and postpartum women are mixed but suggest pregnancy and postpartum periods may heighten risk for some cisgender women. However, research was lacking on pregnant and postpartum TNB people during the pandemic, and further work should examine the impact of pregnancy more inclusively.
Frontline workers
Due to high levels of stress and risks for exposure to COVID-19 for health care and other frontline workers during the pandemic, research on health and health behaviors is important for understanding the broad impacts on this population. Yet, only two studies on frontline workers met inclusion criteria.85,119 Among health care workers in New Orleans, there were no significant gender differences in AUDIT-C scores. However, cisgender men's rates of high-risk drinking (defined as a score of 4 or greater) stayed the same over time (45% at both time points), whereas cisgender women's rates of high-risk drinking were higher during the pandemic compared to pre-pandemic (48% vs. 45%, respectively).85 In another study among health care workers at 25 hospitals, adjusted analyses found that cisgender women were no more likely than cisgender men to have symptoms consistent with probable AUD despite significantly higher likelihood of probable post-traumatic stress disorder (PTSD).119
Coping, Stress, and Mental Health
The literature search yielded 10 studies that analyzed gender differences in alcohol use and also tested associations between stress or mental health and alcohol use during the pandemic.94,100,119-126 However, only five of these studies examined whether the associations between alcohol and stress or mental health differed by gender,94,100,120,121,124 three of which included pre-pandemic data.100,120,124 Two studies demonstrated mixed findings about drinking to cope early in the pandemic among cisgender women.100,120 One study found significant associations between COVID-related stressors and drinking to cope, with stronger associations for cisgender men than cisgender women.120 In the other study, stronger coping motives for drinking were associated with higher drinking levels at baseline for cisgender women, and loneliness and coping were related to changes in drinking levels over time.100
Analyses using data from a quasi-experimental study of a nationally representative sample determined that cisgender women interviewed during the pandemic (compared to cisgender women interviewed pre-pandemic) were nearly 1.5 times more likely to report that drinking helped them forget their worries.124 Among cisgender women, single women (compared to married women) were more likely, and Black women (compared to white women) were less likely to report drinking to forget their worries. Cisgender women with moderate to severe symptoms of depression (compared to no depressive symptoms; adjusted odds ratio: 2.45) and mild symptoms of anxiety (compared to no anxiety symptoms; adjusted odds ratio: 1.62) were significantly more likely to say that drinking helped them cope with their worries.124 There were no differences among cisgender men and no differences in comparisons between cisgender women and cisgender men. Depression and anxiety were associated with heightened risks for alcohol use121 and drinking to cope124 among cisgender women during the pandemic.
TNB Individuals and SMW
TNB populations
Seven studies documented how the COVID-19 pandemic has impacted TNB people's drinking.101,115,127-131 These studies included five cross-sectional and two prospective analyses, primarily began data collection in early pandemic, and all had trans-specific sample sizes of 200 or less. Within the literature that examined the drinking behaviors and trajectories of TNB people following the onset of COVID-19, the referent group to which TNB people were compared varied across studies. In some studies, the comparison was between TNB people and cisgender (or specifically cisgender and heterosexual) peers.128,130,131 In other studies, TNB people were aggregated and compared against cisgender women.115,127,129 One study included solely TNB people and evaluated their current behaviors against their retrospectively reported pre-pandemic behaviors.101
These comparisons provide differing information on TNB people's drinking during the COVID-19 pandemic. Comparisons between TNB people and cisgender women, which were assessed at a variety of pandemic time points, typically found no significant differences between these groups in terms of alcohol use frequency (e.g., number of drinks consumed in a given day), alcohol use changes (e.g., self-reported drinking frequency before and during the pandemic), and likelihood of drinking to cope.115,127,129 For the literature comparing TNB populations to cisgender or cisgender/heterosexual peers more generally, TNB people and cisgender/heterosexual peers had comparable rates of increased drinking during the pandemic (TNB: 10.5%; cisgender/heterosexual: 13%) and were equally likely to exhibit problem drinking (based on PROMIS scores).131
Compared to cisgender men and SMW peers, TNB respondents reported a lower likelihood of problem drinking (using AUDIT),130 even though they reported higher psychological distress during the early pandemic.128 However, based on self-report, TNB respondents were more likely to report substantial increases in drinking during the pandemic. Notably, these results are drawn solely from college students.130
Other research on college students that drew from a more general sample addressed these substantial changes in drinking due to the pandemic, finding that mean number of drinks in the past 30 days among "non-cisgender" people, using the phrasing of that study, rose from 9.2 pre-pandemic (February 2020) to 16.8 during the pandemic (October 2020). However, these levels were lower than among either cisgender men or women peers.101 Extant research on TNB people's drinking during the pandemic yielded conflicting results, with the most common result being null findings of differences between TNB people and cisgender peers across a number of drinking outcomes (though this varied based on the specific comparison being drawn). This small pool of research also lacked examinations of other TNB-specific factors that may influence drinking during the pandemic, such as transphobic experiences or sustained access to trans-related and trans-affirming health care as a preventive measure against psychological distress.
Sexual minority women
Four studies included findings specific to cisgender SMW.127,128,132,133 More SMW than any other group reported self-perceived increases in alcohol use since the start of the pandemic (39% vs. 33% of sexual minority men and 24.5% of cisgender heterosexual women).133 Two of the studies used the same sample but reported on different time points in recruitment (earlier in recruitment132 and after all participants had been recruited127). Among participants who were recruited earlier in the study/pandemic, most reported increased anxiety and depression since before the pandemic (more than 90%), but fewer reported increases in drinking (40% to 55% reported increases in drinking quantity, frequency, or both).132 Increases in anxiety and depression were associated with more alcohol consequences and motivation to drink to cope. In the analysis of the entire sample, participants indicated drinking on 26% of days as compared to using cannabis on 32% of days. On drinking days, participants consumed an average of almost three drinks per day and endorsed coping motives on 57% of drinking days.127 Overall, findings indicate higher incidence of increased alcohol use during the pandemic among sexual minority women compared to cisgender heterosexual women and sexual minority men; these increases were associated with higher risks for poor mental health. Notably, none of the studies reviewed included pre-pandemic data, and only one study was prospective.127 Two studies including sexual identity difference analyses (e.g., bisexual compared to lesbian cisgender women) within sexual minority women found few to no differences.127,128 Three studies included only young adults;127,128,132 only one study included participants from a wider age range (anyone older than age 18 was eligible).133
Discussion
This review of the extant literature suggests that alcohol consumption, and especially reports of alcohol-related problems such as AUD symptoms, increased among adults in the United States during the pandemic. Although not all studies were entirely concordant, many increases in the most serious consequences of alcohol consumption seemed to be concentrated in cisgender women. That said, most studies, especially those representative of the U.S. population, indicate that alcohol consumption and alcohol-related harms remain higher among cisgender men. With respect to different subpopulations, data among young adults suggest that alcohol consumption in this age group declined in the early pandemic, with little evidence for gender differences in the decline. Too few studies have focused on cisgender BIPOC women, frontline workers, and older cisgender women to draw broader conclusions, suggesting a need for more research among these populations that have experienced stark disparities in the impacts of the pandemic.33,42,134-138
In the limited research that examined alcohol use among TNB populations, evidence suggests minimal differences in drinking frequency and other drinking outcomes (e.g., rates of increased drinking) between TNB and cisgender populations, at least when the comparison was between TNB people and either cisgender women or cisgender/heterosexual individuals.115,127,129,131 When compared with sexual minority college students, TNB college students had a lower likelihood of problem drinking (as determined using AUDIT) and a higher likelihood of self-reporting substantial changes in drinking during the pandemic.130 TNB college students exhibited increases in mean number of drinks in the past 30 days over the pandemic, but baseline levels were lower than in cisgender men and women peers.101 However, this body of research would benefit from clearer, more nuanced analyses that disentangle the rich diversity of TNB identities and stratify cisgender people by gender and sexual identity. Further research also is warranted on the specific experiences of TNB college students, as this population exhibited unique patterns. Additionally, research on pandemic drinking trajectories among TNB populations would benefit from a stronger emphasis on trans-specific experiences and stressors that may influence alcohol use; this research should be encouraged as an avenue of further inquiry.
Research among LGBTQ people during the pandemic broadly seems to suggest few to no differences compared with cisgender heterosexual populations.104,139 Notably, however, alcohol use seems to have increased since before the pandemic among sexual minority women,133 and these increases are associated with worsened mental health.127,128 This is an alarming finding given large pre-pandemic disparities in both alcohol use and mental health between sexual minority women and heterosexual women.14,140-145 More research is needed to understand the stressors and mechanisms underlying the higher rates of alcohol use among sexual minority women during the pandemic.
Efforts to combat elevated drinking must account for the complex reasons why people drink. Cisgender women were more likely to drink to help forget worries after (compared to before) the onset of the pandemic,124 and economic stressors—such as pay decreases, difficulty paying bills, or losing one's job during the pandemic—have all been linked to increased drinking among cisgender women.146 Using alcohol as a coping mechanism impacted both TNB populations and cisgender women, as drinking to cope during the pandemic occurred at similar levels for both groups127 and was higher for TNB people and cisgender women than for cisgender heterosexual men.147 Cisgender women also experienced greater levels of unpaid labor (e.g., taking care of family members) during the pandemic, which may have increased stress levels.31,148 This may also be true for TNB people, who have faced distressing economic concerns and impacts52,53,149 as well as reduced access to health care, housing, and social/community support.53-55,150 Pandemic-related stressors may be particularly impactful for cisgender women's drinking,151 but the potential impacts on TNB people's drinking is less clear. Further research is needed to fully articulate any stressors and coping practices unique to TNB populations during the pandemic, such as potential shifts in proximal stress (e.g., anticipated stigma, concealment, or internalized transphobia), which has been linked to problematic alcohol use and drinking to cope.58
Whether the associations between mental health concerns and alcohol use were heightened during the pandemic is under-researched; however, rates of depression and anxiety have increased,22,26,27,152 which may put more people, particularly cisgender women, including SMW and TNB people, at higher risk of problematic alcohol use.
Limitations of the Review
One key limitation of this review is the focus on alcohol; different forms of substance use can co-occur, potentially amplifying associated health risks.80 Research is limited on co-occurring substance use among cisgender women and TNB populations during the COVID-19 pandemic. Future research should address co-occurring substance use among cisgender women, sexual minority populations, and TNB populations to thoroughly examine its impact.
This review focuses solely on peer-reviewed publications, which may have led to a limitation of the research reviewed as only 16% of studies included time points in 2021 and none extended into 2022. Perhaps little research was conducted in 2021 that looked at the continued impacts of the pandemic on alcohol use; alternatively, findings may not yet be available in the peer-reviewed literature. Timing is important as different stages of the pandemic may have influenced population alcohol use heterogeneously; moreover, different geographic locations had discrete experiences of the pandemic. For example, the first case of COVID-19 in the United States was documented in January 2020 in Washington State, and cases were largely concentrated on the west coast until March 2020. Stay-at-home orders began in early to mid-March in some areas (e.g., Puerto Rico, California, New Jersey) whereas some states did not issue them until April (e.g., Iowa, South Carolina, Missouri).153 Many cities and states temporarily suspended bar and restaurant operations in the initial stages of the pandemic, which may have made alcohol less accessible; however, countervailing alcohol policies in many states that eased restrictions on take-out and home delivery of alcohol may have counteracted restrictions on on-premise consumption.154,155 Similarly, stressors associated with the initial stages of the pandemic could have contributed to higher rates of alcohol use compared with later stages of the pandemic. However, the extent to which stress eased as the pandemic continued remains understudied. Moreover, evidence suggests that boredom during the pandemic also may have been associated with increased alcohol use.156,157
Articles rarely mentioned when data collection occurred, much less with enough specificity to ensure it occurred during the pandemic, which made it difficult to screen out articles that collected data prior to 2020. To facilitate screening and identification of articles only looking at alcohol use during the pandemic, the authors made the decision to include "COVID" as part of the search strategy to capture relevant literature in the time available for the review and minimize the potential for not finding relevant studies. It would be beneficial to update this review in the future once more research has been published; however, this review gives a preliminary look at the available evidence.
This review excluded studies conducted outside of the United States, given the great variance in how different countries responded to the pandemic. Indeed, a recent systematic review suggests sizable variance in alcohol use during the pandemic depending on the country.158 This U.S.-centric review limited understanding of alcohol use by cisgender women and TNB people during the pandemic on a broader scale. Anecdotally, it was noted that many papers that examined gender differences or focused on cisgender women's alcohol use were conducted outside of the United States. Future reviews should broaden the search to be inclusive of these important studies. Finally, the review excluded qualitative research, as the focus was on rates of alcohol use rather than on more nuanced findings related to reasons for alcohol use or experiences during the pandemic.
Limitations of the Literature
Among the reviewed literature, the most robust designs were longitudinal, multi-cohort approaches and included pre-pandemic data (e.g., Jaffe et al.107). Pre-pandemic longitudinal data allow for assessment of pandemic-related deviations from existing patterns. For example, college students typically increase alcohol consumption during the spring semester; therefore, increases in alcohol use in spring 2020 during the pandemic period are not atypical and, in fact, might have been lower than expected.107 Another limitation is that most studies did not test for gender-by-time interactions; as a result, there are limited data on whether or not gender differences existed in changes over time. Examination of gender differences was further complicated by a frequent lack of clarity as to whether studies were reporting on sex or gender, or simply reporting on "women" without specifying how many of these women were cisgender or TNB. Generally, if studies did not mention TNB people in their study population, it is likely that TNB status was either not measured or considered, or that TNB people were actively excluded. Thus, in this review, studies that did not discuss gender outside of cisgender women and men, or that only used the terms "women" and "men," were presumed to be not inclusive of TNB people.
Another limitation related to research design is measurement of alcohol use, changes in alcohol use, and other alcohol-related outcomes. Although many studies used validated measures of alcohol problems or commonly used measures of quantity and frequency, others relied on more subjective assessments. For example, 28% of the reviewed studies measured change in alcohol use by asking participants for their perceptions of change since the pandemic's start, and 8% of studies asked participants to retrospectively report drinking levels pre-pandemic and current drinking. Retrospective subjective comparisons of alcohol use before and during the pandemic with unvalidated measures were perhaps necessary given the lack of pre-pandemic data collection in many studies but may have resulted in substantial measurement error. Further, definitions of alcohol use (e.g., problems, binge drinking) varied, making comparisons across studies challenging. Finally, given the heterogeneity of measures employed and domains of alcohol use examined, the current literature is limited in its ability to allow for any kinds of conclusions about differential rates of drinking versus alcohol problems.
Very few studies focused on BIPOC populations, which is particularly troubling given the sizable racial/ethnic disparities in COVID-19 infections and deaths159 and the compounding impacts of sociopolitical events, racism (including anti-Asian hate/attacks), xenophobia, and economic concerns on well-being.160,161 The review also found few studies that included comparisons between cisgender and TNB populations, and those that did lacked sample sizes to conduct subgroup comparisons among TNB people (e.g., transgender men versus transgender women), despite discrete risks.64 TNB populations are underrepresented in gender differences research; thus, more research on alcohol use among TNB people during the pandemic is needed to better understand rates of alcohol use and unique risk factors. Similarly, despite identified high risks among SMW, studies examining LGBTQ subgroups often had extremely small sample sizes for these groups, limiting the capacity for studies to identify significant differences. Few studies reported the intersections between gender and sexual identity (e.g., comparing bisexual men and bisexual women), thus limiting our understanding of gender differences.
No studies looked at gender differences in parenting and how that might be associated with potentially higher risk for alcohol use. Little research examined alcohol use among couples, despite ample research demonstrating partners' impacts on each other's drinking162,163 and clear linkages between intimate partner violence and alcohol,164,165 as well as the increased risks for intimate partner violence during the pandemic.35,36,166
One of the clearest limitations of the literature was the overall lack of research examining gender differences, which may be additionally related to the challenges of doing research during the height of the pandemic. The shift to working from home and the demands of social distancing made in-person research challenging, if not impossible, which had downstream implications for new research recruitment and data collection. Moreover, the pandemic had unequal impacts on the productivity of women and researchers from marginalized groups,167-171 which may have had disproportionate impacts on rates of research focused on cisgender women, BIPOC women, and TNB populations during the pandemic.
Implications
The findings of this review point to a continued need for alcohol-reduction interventions. A discussion of the complexities of cisgender women's and TNB people's treatment utilization is beyond the scope of this review. However, there are unique pandemic-related considerations that may be worth attention. Although the extent to which pandemic-related increases in alcohol consumption will persist over the long term remains unknown, available research from disasters indicates that AUDs exacerbated by disaster exposures can persist over time for some individuals;172 thus, considering alcohol treatment and service capacity and pre-pandemic disparities is warranted. Interventions to reduce alcohol consumption and treat symptoms of AUDs have well-documented efficacy. However, before the pandemic, cisgender women5 and TNB individuals62,67,173 already had diminished rates of service utilization that may have been exacerbated in the pandemic setting. Digitally delivered services may increase access across populations,174,175 yet cisgender women, including SMW, and TNB people have more complex comorbidities that may require higher levels of care.5,67,176,177 For BIPOC women, SMW, and TNB people, treatment also needs to address minority stressors such as discrimination and stigma51,173,178-183 and needs to be intersectional to address the overlapping and compounding impacts of multiple sources of oppression and marginalization.184-187 Thus, an urgent research priority stemming from these findings is to evaluate accessibility and acceptance of service modalities.
There have been calls not to treat mental health concerns or problematic health behaviors as individual-level issues, particularly during a ubiquitous stressful and public health crisis such as a global pandemic.188,189 Instead, interventions should take a public health approach by modifying social and contextual factors to build resiliency.160,190,191 People have multiple motives for drinking, such as cravings192 or enhancing social situations.112 Yet, the unique impacts of pandemic-related stressors warrant enhancing access to resources, both emotional and economic, that may, in turn, help decrease stress- and coping-related motivations to drink. Efforts aimed at reducing distress and lowering risks for problematic alcohol use thus need to focus on ensuring consistent population-level access to resources such as social support, childcare and elder care, sick leave, affordable and accessible health care (including mental health care), affordable and permanent housing, education, living wages, and access to accurate health information. Whether these alone would be sufficient during a pandemic to reduce barriers to accessing help and uniquely support cisgender women and TNB people is unknown.
Further, alcohol policies to reduce access are effective in reducing harm.193 Alcohol policies generally became more permissive during the pandemic (e.g., "to-go" drinks, home delivery). Some of those pandemic-related changes are becoming permanent in some states.194 Revisiting alcohol regulation, including increasing price, as a public health approach could have considerable public health benefits.
Summary of Conclusions
The gender gap in alcohol use is narrowing between cisgender men and women—and seems to have gotten even narrower during the pandemic. Additionally, cisgender women and TNB people are less likely to seek treatment, and there may be unique health risks related to COVID-19 and alcohol use at least for cisgender women. Thus, research, prevention, and intervention efforts are needed to address this public health issue. Halting this worrisome trend in alcohol use by cisgender women—across sexual identities—requires a public health approach that considers the unique needs and concerns of cisgender women. More research also is needed to understand alcohol use by TNB individuals during the pandemic and how to best build resilience and support for this underserved population. Ultimately, this paper is about both sex and gender, capturing the drinking-related experiences of cisgender women (for whom these align) and TNB populations (for whom they do not), as well as various subpopulations that may face unique risks (such as pregnant people). Thus, findings suggest that research on alcohol use and other mental health concerns needs to take both sex and gender (including gender-diverse individuals beyond just comparisons between cisgender men and women) into account to understand not only differences in rates and changes over time but also differences in predictors and outcomes.
Acknowledgments
Dr. Veldhuis' work on this manuscript was partially supported by an NIH/NIAAA Pathway to Independence K99/R00 Award (K99 AA028049; R00 AA028049). The work of Dr. Keyes, Mr. Kreski, and Mr. Usseglio on this manuscript was supported by NIH/NIAAA grant R01 AA026861.
Correspondence
Address correspondence concerning this article to Cindy Veldhuis, Institute for Sexual and Gender Minority Health, 625 North Michigan, Chicago IL 60611. Email: cbv@northwestern.edu
Disclosures
The authors declare no competing financial or nonfinancial interests.
Publisher's note
Opinions expressed in contributed articles do not necessarily reflect the views of the National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health. The U.S. government does not endorse or favor any specific commercial product or commodity. Any trade or proprietary names appearing in Alcohol Research: Current Reviews are used only because they are considered essential in the context of the studies reported herein.
References
- Keyes KM, Jager J, Mal‐Sarkar T, Patrick ME, Rutherford C, Hasin D. Is there a recent epidemic of women's drinking? A critical review of national studies. Alcohol Clin Exp Res. 2019;43(7):1344-1359. https://doi.org/10.1111/acer.14082.
- Grucza RA, Sher KJ, Kerr WC, et al. Trends in adult alcohol use and binge drinking in the early 21st-century United States: A meta-analysis of 6 national survey series. Alcohol Clin Exp Res. 2018;42(10):1939-1950. https://doi.org/10.1111/acer.13859.
- Grant BF, Chou SP, Saha TD, et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911-923. https://doi.org/10.1001/jamapsychiatry.2017.2161.
- Keyes KM, Hatzenbuehler ML, McLaughlin KA, et al. Stigma and treatment for alcohol disorders in the United States. Am J Epidemiol. 2010;172(12):1364-1372. https://doi.org/10.1093/aje/kwq304.
- McCrady BS, Epstein EE, Fokas KF. Treatment interventions for women with alcohol use disorder. Alcohol Res. 2020;40(2):1-18. https://doi.org/10.35946/arcr.v40.2.08.
- Keyes KM, Martins SS, Blanco C, Hasin DS. Telescoping and gender differences in alcohol dependence: New evidence from two national surveys. Am J Psychiatry. 2010;167(8):969-976. https://doi.org/10.1176/appi.ajp.2009.09081161.
- McCabe SE, West BT, Hughes TL, Boyd CJ. Sexual orientation and substance abuse treatment utilization in the United States: Results from a national survey. J Subst Abuse Treat. 2013;44(1):4-12. https://doi.org/10.1016/j.jsat.2012.01.007.
- Weisner C, Schmidt L. Gender disparities in treatment for alcohol problems. JAMA. 1992;268(14):1872-1876. https://doi.org/10.1001/jama.1992.03490140080039.
- Jeong YM, Veldhuis CB, Aranda F, Hughes TL. Racial/ethnic differences in unmet needs for mental health and substance use treatment in a community-based sample of sexual minority women. J Clin Nurs. 2016;25(23-24):3557-3569. https://doi.org/10.1111/jocn.13477.
- Dawson DA, Room R. Towards agreement on ways to measure and report drinking patterns and alcohol-related problems in adult general population surveys: The Skarpö Conference overview. J Subst Abuse. 2000;12(1-2):1-21. https://doi.org/10.1016/s0899-3289(00)00037-7.
- Erol A, Karpyak VM. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug Alcohol Depend. 2015;156:1-13. https://doi.org/10.1016/j.drugalcdep.2015.08.023.
- Drabble LA, Trocki KF, Korcha RA, Klinger JL, Veldhuis CB, Hughes TL. Comparing substance use and mental health outcomes among sexual minority and heterosexual women in probability and non-probability samples. Drug Alcohol Depend. 2018;185:285-292. https://doi.org/10.1016/j.drugalcdep.2017.12.036.
- Hughes TL, Veldhuis CB, Drabble LA, Wilsnack SC. Research on alcohol and other drug (AOD) use among sexual minority women: A global scoping review. PLoSOne. 2020;15(3):e0229869. https://doi.org/10.1371/journal.pone.0229869.
- Karriker-Jaffe KJ, Drabble LA, Li L, et al. Comparing substance use outcomes by sexual identity among women: Differences using propensity score methods. Drug Alcohol Depend. 2022;238:109567. https://doi.org/10.1016/j.drugalcdep.2022.109567.
- Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. 2017 National Survey on Drug Use and Health: Final Analytic File Codebook. Rockville, MD: U.S. Department of Health and Human Services; 2018. https://www.datafiles.samhsa.gov/sites/default/files/field-uploads-protected/studies/NSDUH-2017/NSDUH-2017-datasets/NSDUH-2017-DS0001/NSDUH-2017-DS0001-info/NSDUH-2017-DS0001-info-codebook.pdf.
- Mulia N, Bensley KM. Alcohol-related disparities among women: Evidence and potential explanations. Alcohol Res. 2020;40(2):09. https://doi.org/10.35946/arcr.v40.2.09.
- Mulia N, Schmidt L, Bond J, Jacobs L, Korcha R. Stress, social support and problem drinking among women in poverty. Addiction. 2008;103(8):1283-1293. https://doi.org/10.1111/j.1360-0443.2008.02234.x.
- Davenport MH, Meyer S, Meah VL, Strynadka MC, Khurana R. Moms are not OK: COVID-19 and maternal mental health. Front Glob Womens Health. 2020;1:1. https://doi.org/10.3389/fgwh.2020.00001.
- Lindau ST, Makelarski JA, Boyd K, et al. Change in health-related socioeconomic risk factors and mental health during the early phase of the COVID-19 pandemic: A national survey of U.S. women. J Womens Health (Larchmt). 2021;30(4):502-513. https://doi.org/10.1089/jwh.2020.8879.
- Kolakowsky-Hayner SA, Goldin Y, Kingsley K, et al. Psychosocial impacts of the COVID-19 quarantine: A study of gender differences in 59 countries. Medicina (Kaunas). 2021;57(8):789. https://doi.org/10.3390/medicina57080789.
- Smail EJ, Riehm KE, Veldhuis CB, et al. Associations of household structure and presence of children in the household with mental distress during the early stages of the U.S. COVID-19 pandemic. Fam Syst Health. 2022;40(1):46-59. https://doi.org/10.1037/fsh0000657.
- Veldhuis CB, Nesoff ED, McKowen ALW, et al. Addressing the critical need for long-term mental health data during the COVID-19 pandemic: Changes in mental health from April to September 2020. Prev Med. 2021;146:106465. https://doi.org/10.1016/j.ypmed.2021.106465.
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacology (Berl). 2001;158(4):343-359. https://doi.org/10.1007/s002130100917.
- Fox HC, Sinha R. Sex differences in drug-related stress-system changes: Implications for treatment in substance-abusing women. Harv Rev Psychiatry. 2009;17(2):103-119. https://doi.org/10.1080/10673220902899680.
- Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. 2008;1141:105-130. https://doi.org/10.1196/annals.1441.030.
- Holingue C, Kalb LG, Riehm KE, et al. Mental distress in the United States at the beginning of the COVID-19 pandemic. Am J Public Health. 2020;110(11):1628-1634. https://doi.org/10.2105/AJPH.2020.305857.
- Riehm KE, Holingue C, Smail EJ, et al. Trajectories of mental distress among U.S. adults during the COVID-19 pandemic. Ann Behav Med. 2021;55(2):93-102. https://doi.org/10.1093/abm/kaaa126.
- Almeida M, Shrestha AD, Stojanac D, Miller LJ. The impact of the COVID-19 pandemic on women's mental health. Arch Womens Ment Health. 2020;23(6):741-748. https://doi.org/10.1007/s00737-020-01092-2.
- Chen JH. Disparities in mental health and well-being between heterosexual and sexual minority older adults during the COVID-19 pandemic. J Aging Health. 2022;34(6-8):939-950. https://doi.org/10.1177/08982643221081965.
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet. 2020;395(10227):912-920. https://doi.org/10.1016/S0140-6736(20)30460-8.
- Connor J, Madhavan S, Mokashi M, et al. Health risks and outcomes that disproportionately affect women during the Covid-19 pandemic: A review. Soc Sci Med. 2020;266:113364. https://doi.org/10.1016/j.socscimed.2020.113364.
- Thibaut F, van Wijngaarden-Cremers PJM. Women's mental health in the time of Covid-19 pandemic. Front Glob Womens Health. 2020;1:588372. https://doi.org/10.3389/fgwh.2020.588372.
- Ornelas IJ, Tornberg-Belanger S, Balkus JE, et al. Coping with COVID-19: The impact of the pandemic on Latina immigrant women's mental health and well-being. Health Educ Behav. 2021;48(6):733-738. https://doi.org/10.1177/10901981211050638.
- Glowacz F, Dziewa A, Schmits E. Intimate partner violence and mental health during lockdown of the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(5):2535. https://doi.org/10.3390/ijerph19052535.
- Gresham AM, Peters BJ, Karantzas G, Cameron LD, Simpson JA. Examining associations between COVID-19 stressors, intimate partner violence, health, and health behaviors. J Soc Pers Relat. 2021;38(8):2291-2307. https://doi.org/10.1177/02654075211012098.
- Lyons M, Brewer G. Experiences of intimate partner violence during lockdown and the COVID-19 pandemic. J Fam Violence. 2022;37(6):969-977. https://doi.org/10.1007/s10896-021-00260-x.
- Parrott DJ, Halmos MB, Stappenbeck CA, Moino K. Intimate partner aggression during the COVID-19 pandemic: Associations with stress and heavy drinking. Psychol Violence. 2022;12(2):95-103. https://doi.org/10.1037/vio0000395.
- Piquero AR, Jennings WG, Jemison E, Kaukinen C, Knaul FM. Domestic violence during the COVID-19 pandemic - Evidence from a systematic review and meta-analysis. J Crim Justice. 2021;74:101806. https://doi.org/10.1016/j.jcrimjus.2021.101806.
- Papautsky EL, Rice DR, Ghoneima H, et al. Characterizing health care delays and interruptions in the United States during the COVID-19 pandemic: Internet-based, cross-sectional survey study. J Med Internet Res. 2021;23(5):e25446. https://doi.org/10.2196/25446.
- Verger NB, Urbanowicz A, Shankland R, McAloney-Kocaman K. Coping in isolation: Predictors of individual and household risks and resilience against the COVID-19 pandemic. Social Sciences & Humanities Open. 2021;3(1):100123. https://doi.org/10.1016/j.ssaho.2021.100123.
- Platt C. Emotional and psychological distress related to COVID-19 isolation, quarantine, and physical distancing: Evidence of gender-based differences. Journal of Research in Gender Studies. 2020;10(2):63-72. https://doi.org/10.22381/JRGS10220202.
- Thomas AS, Osbourne M, Appelhans BM, Roisman GI, Booth‐LaForce C, Bleil ME. Disparities in COVID‐19–related stressful life events in the United States: Understanding who is most impacted. Health Soc Care Community. 2022;30(3):1199-1211. https://doi.org/10.1111/hsc.13671.
- Juster RP, Seeman T, McEwen BS, et al. Social inequalities and the road to allostatic load: From vulnerability to resilience. In: Cicchetti D, ed. Developmental Psychopathology. John Wiley & Sons, Inc.; 2016:1-54. https://doi.org/10.1002/9781119125556.devpsy408.
- Sandifer PA, Juster RP, Seeman TE, Lichtveld MY, Singer BH. Allostatic load in the context of disasters. Psychoneuroendocrinology. 2022;140:105725. https://doi.org/10.1016/j.psyneuen.2022.105725.
- McCaul ME, Roach D, Hasin DS, Weisner C, Chang G, Sinha R. Alcohol and women: A brief overview. Alcohol Clin Exp Res. 2019;43(5):774-779. https://doi.org/10.1111/acer.13985.
- Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943-951. https://doi.org/10.2105/AJPH.2013.301241.
- Bradford NJ, Catalpa JM. Social and psychological heterogeneity among binary transgender, non-binary transgender and cisgender individuals. Psychology & Sexuality. 2019;10(1):69-82. https://doi.org/10.1080/19419899.2018.1552185.
- White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222-231. https://doi.org/10.1016/j.socscimed.2015.11.010.
- Lenning E, Buist CL. Social, psychological and economic challenges faced by transgender individuals and their significant others: Gaining insight through personal narratives. Cult Health Sex. 2013;15(1):44-57. https://doi.org/10.1080/13691058.2012.738431.
- Veldhuis CB, Drabble L, Riggle EDB, Wootton AR, Hughes TL. "I fear for my safety, but want to show bravery for others": Violence and discrimination concerns among transgender and gender-nonconforming individuals after the 2016 presidential election. Violence and Gender. 2018;5(1):26-36. https://doi.org/10.1089/vio.2017.0032.
- Connolly D, Gilchrist G. Prevalence and correlates of substance use among transgender adults: A systematic review. Addict Behav. 2020;111:106544. https://doi.org/10.1016/j.addbeh.2020.106544.
- Ahmed T, Lebbos TJ, Howell S, Lamontagne E, Wimpey JS. Impacts of COVID-19 on the income and mental well-being of cismen, ciswomen, transgender, and non-binary individuals: Evidence from the 2020 COVID-19 Disparities Survey. No. 10184, Policy Research Working Paper Series, The World Bank; 2022. https://doi.org/10.1596/1813-9450-10184.
- Jarrett BA, Peitzmeier SM, Restar A, et al. Gender-affirming care, mental health, and economic stability in the time of COVID-19: A multi-national, cross-sectional study of transgender and nonbinary people. PLoS One. 2021;16(7):e0254215. https://doi.org/10.1371/journal.pone.0254215.
- Felt D, Xu J, Floresca YB, et al. Instability in housing and medical care access: The inequitable impacts of the COVID-19 pandemic on U.S. transgender populations. Transgend Health. 2023;8(1):74-83. https://doi.org/10.1089/trgh.2021.0129.
- Kidd JD, Jackman KB, Barucco R, et al. Understanding the impact of the COVID-19 pandemic on the mental health of transgender and gender nonbinary individuals engaged in a longitudinal cohort study. J Homosex. 2021;68(4):592-611. https://doi.org/10.1080/00918369.2020.1868185.
- Jones BA, Bowe M, McNamara N, Guerin E, Carter T. Exploring the mental health experiences of young trans and gender diverse people during the Covid-19 pandemic. Int J Transgend Health. 2021;24(3):292-304. https://doi.org/10.1080/26895269.2021.1890301.
- O'Handley B, Courtice EL. Mental well-being, social support, and the unique experiences of transgender and nonbinary people during the COVID-19 pandemic. Canadian Journal of Human Sexuality. 2022;31(2):163-175. https://doi.org/10.3138/cjhs.2022-0024.
- Lindley L, Bauerband L, Galupo MP. Using a comprehensive proximal stress model to predict alcohol use. Transgend Health. 2021;6(3):164-174. https://doi.org/10.1089/trgh.2020.0042.
- Lindley L, Bauerband L. The mediating role of avoidant and facilitative coping on the relation between discrimination and alcohol use among transgender and gender-diverse individuals. Transgend Health. Published online July 1, 2022. https://doi.org/10.1089/trgh.2021.0173.
- Blosnich JR, Lehavot K, Glass JE, Williams EC. Differences in alcohol use and alcohol-related health care among transgender and nontransgender adults: Findings from the 2014 Behavioral Risk Factor Surveillance System. J Stud Alcohol Drugs. 2017;78(6):861-866. https://doi.org/10.15288/jsad.2017.78.861.
- Cotaina M, Peraire M, Boscá M, Echeverria I, Benito A, Haro G. Substance use in the transgender population: A meta-analysis. Brain Sci. 2022;12(3):366. https://doi.org/10.3390/brainsci12030366.
- Gilbert PA, Pass LE, Keuroghlian AS, Greenfield TK, Reisner SL. Alcohol research with transgender populations: A systematic review and recommendations to strengthen future studies. Drug Alcohol Depend. 2018;186:138-146. https://doi.org/10.1016/j.drugalcdep.2018.01.016.
- Reisner SL, Hughto JMW. Comparing the health of non-binary and binary transgender adults in a statewide non-probability sample. PLoS One. 2019;14(8):e0221583. https://doi.org/10.1371/journal.pone.0221583.
- Barger BT, Obedin-Maliver J, Capriotti MR, Lunn MR, Flentje A. Characterization of substance use among underrepresented sexual and gender minority participants in the Population Research in Identity and Disparities for Equality (PRIDE) Study. Subst Abuse. 2021;42(1):104-115. https://doi.org/10.1080/08897077.2019.1702610.
- Coulter RWS, Blosnich JR, Bukowski LA, Herrick AL, Siconolfi DE, Stall RD. Differences in alcohol use and alcohol-related problems between transgender- and nontransgender-identified young adults. Drug Alcohol Depend. 2015;154:251-259. https://doi.org/10.1016/j.drugalcdep.2015.07.006.
- Kidd JD, Jackman KB, Wolff M, Veldhuis CB, Hughes TL. Risk and protective factors for substance use among sexual and gender minority youth: A scoping review. Curr Addict Rep. 2018;5(2):158-173. https://doi.org/10.1007/s40429-018-0196-9.
- Keuroghlian AS, Reisner SL, White JM, Weiss RD. Substance use and treatment of substance use disorders in a community sample of transgender adults. Drug Alcohol Depend. 2015;152:139-146. https://doi.org/10.1016/j.drugalcdep.2015.04.008.
- Lombardi E. Substance use treatment experiences of transgender/transsexual men and women. J LGBT Health Res. 2007;3(2):37-47. https://doi.org/10.1300/J463v03n02_05.
- Lombardi EL, van Servellen G. Building culturally sensitive substance use prevention and treatment programs for transgendered populations. J Subst Abuse Treat. 2000;19(3):291-296. https://doi.org/10.1016/S0740-5472(00)00114-8.
- Kidd JD, Paschen-Wolff MM, Mericle AA, Caceres BA, Drabble LA, Hughes TL. A scoping review of alcohol, tobacco, and other drug use treatment interventions for sexual and gender minority populations. J Subst Abuse Treat. 2022;133:108539. https://doi.org/10.1016/j.jsat.2021.108539.
- Oberheim ST, DePue MK, Hagedorn WB. Substance use disorders (SUDs) in transgender communities: The need for trans-competent SUD counselors and facilities. Journal of Addictions & Offender Counseling. 2017;38(1):33-47. https://doi.org/10.1002/jaoc.12027.
- Glynn TR, van den Berg JJ. A systematic review of interventions to reduce problematic substance use among transgender individuals: A call to action. Transgend Health. 2017;2(1):45-59. https://doi.org/10.1089/trgh.2016.0037.
- Coulter RWS, Egan JE, Kinsky S, et al. Mental health, drug, and violence interventions for sexual/gender minorities: A systematic review. Pediatrics. 2019;144(3):e20183367. https://doi.org/10.1542/peds.2018-3367.
- Bailey KL, Sayles H, Campbell J, et al. COVID‐19 patients with documented alcohol use disorder or alcohol‐related complications are more likely to be hospitalized and have higher all‐cause mortality. Alcohol Clin Exp Res. 2022;46(6):1023-1035. https://doi.org/10.1111/acer.14838.
- Larson PS, Bergmans RS. Impact of the COVID-19 pandemic on temporal patterns of mental health and substance abuse related mortality in Michigan: An interrupted time series analysis. Lancet Reg Health Am. 2022;10:100218. https://doi.org/10.1016/j.lana.2022.100218.
- Yeo YH, He X, Ting PS, et al. Evaluation of trends in alcohol use disorder–related mortality in the US before and during the COVID-19 pandemic. JAMA Netw Open. 2022;5(5):e2210259. https://doi.org/10.1001/jamanetworkopen.2022.10259.
- Wang QQ, Kaelber DC, Xu R, Volkow ND. COVID-19 risk and outcomes in patients with substance use disorders: Analyses from electronic health records in the United States. Mol Psychiatry. 2021;26(1):30-39. https://doi.org/10.1038/s41380-020-00880-7.
- Sohal A, Khalid S, Green V, Gulati A, Roytman M. The pandemic within the pandemic: Unprecedented rise in alcohol-related hepatitis during the COVID-19 pandemic. J Clin Gastroenterol. 2022;56(3):e171-e175. https://doi.org/10.1097/MCG.0000000000001627.
- Chandran K, Mazer-Amirshahi M, Shankar N, Desale S, Nelson L, Mete M. Impact of COVID-19 pandemic on emergency department substance use screens and overdose presentations. Am J Emerg Med. 2021;50:472-476. https://doi.org/10.1016/j.ajem.2021.08.058.
- Kumar N, Janmohamed K, Nyhan K, et al. Substance, use in relation to COVID-19: A scoping review. Addict Behav. 2022;127:107213. https://doi.org/10.1016/j.addbeh.2021.107213.
- Dobbins M. Steps for Conducting a Rapid Review. National Collaborating Centre for Methods and Tools; 2017. https://www.nccmt.ca/uploads/media/media/0001/01/a816af720e4d587e13da6bb307df8c907a5dff9a.pdf.
- Ganann R, Ciliska D, Thomas H. Expediting systematic reviews: Methods and implications of rapid reviews. Implement Sci. 2010;5:56. https://doi.org/10.1186/1748-5908-5-56.
- Tricco AC, Langlois EV, Straus SE, eds. Rapid Reviews to Strengthen Health Policy and Systems: A Practical Guide. World Health Organization; 2017. https://ahpsr.who.int/docs/librariesprovider11/publications/supplementa….
- Acharya B, Dhakal C. Risky health behaviors during the COVID-19 pandemic: Evidence from the expenditures on alcohol, non-alcoholic beverages, and tobacco products. PLoS One. 2022;17(5):1-14. https://doi.org/10.1371/journal.pone.0268068.
- Beiter KJ, Wiedemann RP, Thomas CL, Conrad EJ. Alcohol consumption and COVID-19–related stress among health care workers: The need for continued stress-management interventions. Public Health Rep. 2022;137(2):326-335. https://doi.org/10.1177/00333549211058176.
- Boschuetz N, Cheng S, Mei L, Loy VM. Changes in alcohol use patterns in the United States during COVID-19 pandemic. WMJ. 2020;119(3):171-176.
- Capasso A, Jones AM, Ali SH, Foreman J, Tozan Y, DiClemente RJ. Increased alcohol use during the COVID-19 pandemic: The effect of mental health and age in a cross-sectional sample of social media users in the U.S. Prev Med. 2021;145:1-7. https://doi.org/10.1016/j.ypmed.2021.106422.
- Grossman ER, Benjamin-Neelon SE, Sonnenschein S. Alcohol consumption during the COVID-19 pandemic: A cross-sectional survey of US adults. Int J Environ Res Public Health. 2020;17(24):1-10. https://doi.org/10.3390/ijerph17249189.
- Kerr WC, Ye Y, Martinez P, et al. Longitudinal assessment of drinking changes during the pandemic: The 2021 COVID‐19 follow‐up study to the 2019 to 2020 National Alcohol Survey. Alcohol Clin Exp Res. 2022;46(6):1050-1061. https://doi.org/10.1111/acer.14839.
- Knell G, Robertson MC, Dooley EE, Burford K, Mendez KS. Health behavior changes during COVID-19 pandemic and subsequent "stay-at-home" orders. Int J Environ Res Public Health. 2020;17(17):6268. https://doi.org/10.3390/ijerph17176268.
- Walia N, Bhetuwal R, Acosta L, et al. Employment status and its association with psychological distress and alcohol consumption. Cureus. 2021;13(6):1-9. https://doi.org/10.7759/cureus.16054.
- Chartier KG, Guidry JPD, Lee CA, Buckley TD. At home and online during the early months of the COVID-19 pandemic and the relationship to alcohol consumption in a national sample of U.S. adults. PLoS One. 2021;16(11):e0259947. https://doi.org/10.1371/journal.pone.0259947.
- French MT, Mortensen K, Timming AR. Changes in self-reported health, alcohol consumption, and sleep quality during the COVID-19 pandemic in the United States. Applied Economics Letters. 2022;29(3):219-225. https://doi.org/10.1080/13504851.2020.1861197.
- Lannoy S, Fama R, Sassoon SA, et al. A prospective study revealing a compounded burden of COVID-19, sex, and clinical diagnosis of alcohol use disorder and HIV infection on quality of life, anxiety, and alcohol use. J Psychiatr Res. 2022;152:152-159. https://doi.org/10.1016/j.jpsychires.2022.06.017.
- Leventhal AM, Cho J, Ray LA, et al. Alcohol use trajectories among U.S. adults during the first 42 weeks of the COVID‐19 pandemic. Alcohol Clin Exp Res. 2022;46(6):1062-1072. https://doi.org/10.1111/acer.14824.
- Meanley S, Choi SK, Thompson AB, et al. Short-term binge drinking, marijuana, and recreational drug use trajectories in a prospective cohort of people living with HIV at the start of COVID-19 mitigation efforts in the United States. Drug Alcohol Depend. 2022;231:1-9. https://doi.org/10.1016/j.drugalcdep.2021.109233.
- Nordeck CD, Riehm KE, Smail EJ, et al. Changes in drinking days among United States adults during the COVID‐19 pandemic. Addiction. 2022;117(2):331-340. https://doi.org/10.1111/add.15622.
- Osaghae I, Nguyen LK, Chung TH, et al. Prevalence and factors associated with mental health symptoms in adults undergoing Covid-19 testing. J Prim Care Community Health. 2021;12:1-10. https://doi.org/10.1177/21501327211027100.
- Pollard MS, Tucker JS, Green HD, Jr. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. 2020;3(9):e2022942. https://doi.org/10.1001/jamanetworkopen.2020.22942.
- Tucker JS, Rodriguez A, Green HD, Jr., Pollard MS. Trajectories of alcohol use and problems during the COVID-19 pandemic: The role of social stressors and drinking motives for men and women. Drug Alcohol Depend. 2022;232:10925. https://doi.org/10.1016/j.drugalcdep.2022.109285.
- Coakley KE, Lardier DT, Holladay KR, Amorim FT, Mechler H, Zuhl MN. Mental health severity is associated with increases in alcohol consumption in young adult students during the COVID-19 pandemic. Alcohol Treat Q. 2021;39(3):328-341. https://doi.org/10.1080/07347324.2021.1917325.
- Hill EM, Ruark R. An examination of the role of social comparison orientation and social norms in drunkorexia engagement. Addict Behav. 2022;124:107107. https://doi.org/https://doi.org/10.1016/j.addbeh.2021.107107.
- Kim H, Rackoff GN, Fitzsimmons-Craft EE, et al. College mental health before and during the COVID-19 pandemic: Results from a nationwide survey. Cognit Ther Res. 2022;46(1):1-10. https://doi.org/10.1007/s10608-021-10241-5.
- Schwartz SE, Ross SG, Bryant JA, Duncan JD. Mental and physical health among students at a private university that held in-person classes during the COVID-19 pandemic. J Am Coll Health. Published online March 17, 2022:1-11. https://doi.org/10.1080/07448481.2022.2052074.
- Brener ND, Bohm MK, Jones CM, et al. Use of tobacco products, alcohol, and other substances among high school students during the COVID-19 pandemic — Adolescent Behaviors and Experiences Survey, United States, January–June 2021. MMWR Suppl. 2022;71(3):8-15. https://doi.org/10.15585/mmwr.su7103a2.
- Graupensperger S, Fleming CB, Jaffe AE, Rhew IC, Patrick ME, Lee CM. Changes in young adults' alcohol and marijuana use, norms, and motives from before to during the COVID-19 pandemic. J Adolesc Health. 2021;68(4):658-665. https://doi.org/10.1016/j.jadohealth.2021.01.008.
- Jaffe AE, Kumar SA, Ramirez JJ, DiLillo D. Is the COVID‐19 pandemic a high‐risk period for college student alcohol use? A comparison of three spring semesters. Alcohol Clin Exp Res. 2021;45(4):854-863. https://doi.org/10.1111/acer.14572.
- Miech R, Patrick ME, Keyes K, O'Malley PM, Johnston L. Adolescent drug use before and during U.S. national COVID-19 social distancing policies. Drug Alcohol Depend. 2021;226:108822. https://doi.org/10.1016/j.drugalcdep.2021.108822.
- Romm KF, Patterson B, Arem H, Price OA, Wang Y, Berg CJ. Cross-sectional retrospective assessments versus longitudinal prospective assessments of substance use change among young adults during COVID-19: Magnitude and correlates of discordant findings. Subst Use Misuse. 2022;57(3):484-489. https://doi.org/10.1080/10826084.2021.2012696.
- Romm KF, Patterson B, Wysota CN, Wang Y, Berg CJ. Predictors of negative psychosocial and health behavior impact of COVID-19 among young adults. Health Educ Res. 2022;36(4):385-397. https://doi.org/10.1093/her/cyab026.
- Ryerson NC, Wilson OWA, Pena A, Duffy M, Bopp M. What happens when the party moves home? The effect of the COVID-19 pandemic on U.S. college student alcohol consumption as a function of legal drinking status using longitudinal data. Transl Behav Med. 2021;11(3):772-774. https://doi.org/10.1093/tbm/ibab006.
- Stevenson BL, Parks MJ, Patrick ME. Daily associations between affect, drinking motives, and drinking intensity among U.S. young adults. Psychol Addict Behav. 2023;37(2):275-284. https://doi.org/10.1037/adb0000809.
- Eastman MR, Finlay JM, Kobayashi LC. Alcohol use and mental health among older American adults during the early months of the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18(8):4222. https://doi.org/10.3390/ijerph18084222.
- Hanson JD, Noonan C, Harris A, et al. Alcohol consumption during COVID among women with an existing alcohol-use disorder. Int J Environ Res Public Health. 2021;18(18):9460. https://doi.org/10.3390/ijerph18189460.
- Hicks TA, Chartier KG, Buckley TD, et al. Divergent changes: Abstinence and higher-frequency substance use increase among racial/ethnic minority young adults during the COVID-19 global pandemic. Am J Drug Alcohol Abuse. 2022;48(1):88-99. https://doi.org/10.1080/00952990.2021.1995401.
- Ahlers-Schmidt CR, Hervey AM, Neil T, Kuhlmann S, Kuhlmann Z. Concerns of women regarding pregnancy and childbirth during the COVID-19 pandemic. Patient Educ Couns. 2020;103(12):2578-2582. https://doi.org/10.1016/j.pec.2020.09.031.
- McMillan IF, Armstrong LM, Langhinrichsen-Rohling J. Transitioning to parenthood during the pandemic: COVID-19 related stressors and first-time expectant mothers' mental health. Couple and Family Psychology: Research and Practice. 2021;10(3):179-189. https://doi.org/10.1037/cfp0000174.
- Rodriguez LM, Litt DM, Stewart SH. COVID-19 psychological and financial stress and their links to drinking: A dyadic analysis in romantic couples. Psychol Addict Behav. 2021;35(4):377-390. https://doi.org/10.1037/adb0000724.
- Hennein R, Mew EJ, Lowe SR. Socio-ecological predictors of mental health outcomes among healthcare workers during the COVID-19 pandemic in the United States. PLoS One. 2021;16(2):1-18. https://doi.org/10.1371/journal.pone.0246602.
- Cummings JR, Ackerman JM, Wolfson JA, Gearhardt AN. COVID-19 stress and eating and drinking behaviors in the United States during the early stages of the pandemic. Appetite. 2021;162: 105163. https://doi.org/10.1016/j.appet.2021.105163.
- Devoto A, Himelein-Wachowiak M, Liu T, Curtis B. Women's substance use and mental health during the COVID-19 pandemic. Womens Health Issues. 2022;32(3):235-240. https://doi.org/10.1016/j.whi.2022.01.004.
- Graupensperger S, Cadigan JM, Einberger C, Lee CM. Multifaceted COVID-19-related stressors and associations with indices of mental health, well-being, and substance use among young adults. Int J Ment Health Addict. 2023;21(1):418-431. https://doi.org/10.1007/s11469-021-00604-0.
- Helminen EC, Scheer JR, Jackson SD, et al. PTSD symptoms and hazardous drinking indicators among trauma-exposed sexual minority women during heightened societal stress. Behav Med. 2023;49(2):183-194. https://doi.org/10.1080/08964289.2021.2006132.
- Martinez P, Karriker-Jaffe KJ, Ye Y, et al. Mental health and drinking to cope in the early COVID period: Data from the 2019–2020 US National Alcohol Survey. Addict Behav. 2022;128:107247. https://doi.org/10.1016/j.addbeh.2022.107247.
- Nesoff ED, Gutkind S, Sirota S, McKowen AL, Veldhuis CB. Mental health and economic stressors associated with high-risk drinking and increased alcohol consumption early in the COVID-19 pandemic in the United States. Prev Med. 2021;153:106854. https://doi.org/10.1016/j.ypmed.2021.106854.
- Vogel EA, Chieng A, Robinson A, Pajarito S, Prochaska JJ. Associations between substance use problems and stress during COVID-19. J Stud Alcohol Drugs. 2021;82(6):776-781. https://doi.org/10.15288/jsad.2021.82.776.
- Dyar C, Crosby S, Newcomb ME, Mustanski B, Kaysen D. Doomscrolling: Prospective associations between daily COVID news exposure, internalizing symptoms, and substance use among sexual and gender minority individuals assigned female at birth. Psychology of Sexual Orientation and Gender Diversity. Published online May 26, 2022. https://doi.org/10.1037/sgd0000585.
- Salerno JP, Shrader CH, Algarin AB, Lee JY, Fish JN. Changes in alcohol use since the onset of COVID-19 are associated with psychological distress among sexual and gender minority university students in the U.S. Drug Alcohol Depend. 2021;221:108594. https://doi.org/10.1016/j.drugalcdep.2021.108594.
- Sumetsky N, Frankeberger J, Coulter RWS, Burke JG, Friedman MR, Mair C. Mental health and alcohol use during and before the early phases of the COVID-19 pandemic. Behav Med. 2023;49(2):195-203. https://doi.org/10.1080/08964289.2021.2015278.
- Zhang Y, Farina RE, Lawrence SE, et al. How social support and parent–child relationship quality relate to LGBTQ+ college students' well-being during COVID-19. J Fam Psychol. 2022;36(5):653-660. https://doi.org/10.1037/fam0000981.
- Akré ER, Anderson A, Stojanovski K, Chung KW, VanKim NA, Chae DH. Depression, anxiety, and alcohol use among LGBTQ+ people during the COVID-19 pandemic. Am J Public Health. 2021;111(9):1610-1619. https://doi.org/10.2105/AJPH.2021.306394.
- Dyar C, Morgan E, Kaysen D, Newcomb ME, Mustanski B. Risk factors for elevations in substance use and consequences during the COVID-19 pandemic among sexual and gender minorities assigned female at birth. Drug Alcohol Depend. 2021;227:109015. https://doi.org/10.1016/j.drugalcdep.2021.109015.
- Peterson ZD, Vaughan EL, Carver DN. Sexual identity and psychological reactions to COVID-19. Traumatology. 2021;27(1):6-13. https://doi.org/10.1037/trm0000283.
- Bassett MT, Chen JT, Krieger N. Variation in racial/ethnic disparities in COVID-19 mortality by age in the United States: A cross-sectional study. PLoS Med. 2020;17(10):e1003402. https://doi.org/10.1371/journal.pmed.1003402.
- Froessl LJ, Abdeen Y. The silent pandemic: The psychological burden on frontline healthcare workers during COVID-19. Psychiatry J. 2021:1-11. https://doi.org/10.1155/2021/2906785.
- Gouda D, Singh PM, Gouda P, Goudra B. An overview of health care worker reported deaths during the COVID-19 pandemic. J Am Board Fam Med. 2021;34(Suppl):S244-S246. https://doi.org/10.3122/jabfm.2021.S1.200248.
- Wortham JM, Lee JT, Althomsons S, et al. Characteristics of persons who died with COVID-19 - United States, February 12-May 18, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(28):923-929. https://doi.org/10.15585/mmwr.mm6928e1.
- Martínez ME, Nodora JN, Carvajal‐Carmona LG. The dual pandemic of COVID‐19 and systemic inequities in US Latino communities. Cancer. 2021;127(10):1548-1550. https://doi.org/10.1002/cncr.33401.
- Gattamorta KA, Salerno J, Islam JY, Vidot DC. Mental health among LGBTQ cannabis users during the COVID-19 pandemic: Analysis of the COVID-19 Cannabis Health Study. Psychol Sex Orientat Gend Divers. 2021;8(2):172-179. https://doi.org/10.1037/sgd0000491.
- Blosnich JR, Nasuti LJ, Mays VM, Cochran SD. Suicidality and sexual orientation: Characteristics of symptom severity, disclosure, and timing across the life course. Am J Orthopsychiatry. 2016;86(1):69-78. https://doi.org/10.1037/ort0000112.
- Bostwick WB, Boyd CJ, Hughes TL, McCabe SE. Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. Am J Public Health. 2010;100(3):468-475. https://doi.org/10.2105/AJPH.2008.152942.
- Fredriksen Goldsen KI, Jen S, Muraco A. Iridescent Life Course: LGBTQ aging research and blueprint for the future – A systematic review. Gerontology. 2019;65(3):253-274. https://doi.org/10.1159/000493559.
- Jorm AF, Korten AE, Rodgers B, Jacomb PA, Christensen H. Sexual orientation and mental health: Results from a community survey of young and middle-aged adults. Br J Psychiatry. 2002;180(5):423-427. https://doi.org/10.1192/bjp.180.5.423.
- McCabe SE, Hughes TL, West BT, Veliz P, Boyd CJ. DSM-5 alcohol use disorder severity as a function of sexual orientation discrimination: A national study. Alcohol Clin Exp Res. 2019;43(3):497-508. https://doi.org/10.1111/acer.13960.
- Talley AE, Hughes TL, Aranda F, Birkett M, Marshal MP. Exploring alcohol-use behaviors among heterosexual and sexual minority adolescents: Intersections with sex, age, and race/ethnicity. Am J Public Health. 2014;104(2):295-303. https://doi.org/10.2105/AJPH.2013.301627.
- Sampson L, Ettman CK, Abdalla SM, et al. Financial hardship and health risk behavior during COVID-19 in a large US national sample of women. SSM Popul Health. 2021;13:100734. https://doi.org/10.1016/j.ssmph.2021.100734.
- Krueger EA, Barrington-Trimis JL, Unger JB, Leventhal AM. Sexual and gender minority young adult coping disparities during the COVID-19 pandemic. J Adolesc Health. 2021;69(5):746-753. https://doi.org/10.1016/j.jadohealth.2021.07.021.
- Power K. The COVID-19 pandemic has increased the care burden of women and families. Sustainability: Science, Practice and Policy. 2020;16(1):67-73. https://doi.org/10.1080/15487733.2020.1776561.
- Carpenter CS, Eppink ST, Gonzales G. Transgender status, gender identity, and socioeconomic outcomes in the United States. ILR Review. 2020;73(3):573-599. https://doi.org/10.1177/0019793920902776.
- Restar AJ, Jin H, Jarrett B, et al. Characterising the impact of COVID-19 environment on mental health, gender affirming services and socioeconomic loss in a global sample of transgender and non-binary people: A structural equation modelling. BMJ Glob Health. 2021;6(3):e004424. https://doi.org/10.1136/bmjgh-2020-004424.
- Rodriguez LM, Litt DM, Stewart SH. Drinking to cope with the pandemic: The unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav. 2020;110:106532. https://doi.org/10.1016/j.addbeh.2020.106532.
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020;3(9):e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686.
- Moreland A, Herlihy C, Tynan MA, et al. Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement - United States, March 1-May 31, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(35):1198-1203. https://doi.org/10.15585/mmwr.mm6935a2.
- Rehm J, Kilian C, Ferreira‐Borges C, et al. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug Alcohol Rev. 2020;39(4):301-304. https://doi.org/10.1111/dar.13074.
- Leung JYY, Au Yeung SL, Lam TH, Casswell S. What lessons does the COVID-19 pandemic hold for global alcohol policy? BMJ Glob Health. 2021;6(7):e006875. https://doi.org/10.1136/bmjgh-2021-006875.
- Weiss ER, Todman M, Maple E, Bunn RR. Boredom in a time of uncertainty: State and trait boredom's associations with psychological health during COVID-19. Behav Sci (Basel). 2022;12(8):298. https://doi.org/10.3390/bs12080298.
- Patrick ME, Terry-McElrath YM, Miech RA, Keyes KM, Jager J, Schulenberg JE. Alcohol use and the COVID-19 pandemic: Historical trends in drinking, contexts, and reasons for use among U.S. adults. Soc Sci Med. 2022;301:114887. https://doi.org/10.1016/j.socscimed.2022.114887.
- Sohi I, Chrystoja BR, Rehm J, et al. Changes in alcohol use during the COVID‐19 pandemic and previous pandemics: A systematic review. Alcohol Clin Exp Res. 2022;46(4):498-513. https://doi.org/10.1111/acer.14792.
- Kim SJ, Bostwick W. Social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ Behav. 2020;47(4):509-513. https://doi.org/10.1177/1090198120929677.
- Parenteau AM, Boyer CJ, Campos LJ, et al. A review of mental health disparities during COVID-19: Evidence, mechanisms, and policy recommendations for promoting societal resilience. Dev Psychopathol. 2022:1-22. https://doi.org/10.1017/S0954579422000499.
- Garcini LM, Rosenfeld J, Kneese G, Bondurant RG, Kanzler KE. Dealing with distress from the COVID‐19 pandemic: Mental health stressors and coping strategies in vulnerable Latinx communities. Health Soc Care Community. 2022;30(1):284-294. https://doi.org/10.1111/hsc.13402.
- Reczek C, Liu H, Spiker R. A population-based study of alcohol use in same-sex and different-sex unions. J Marriage Fam. 2014;76(3):557-572. https://doi.org/10.1111/jomf.12113.
- Leonard KE, Eiden RD. Marital and family processes in the context of alcohol use and alcohol disorders. Annu Rev Clin Psychol. 2007;3(1):285-310. https://doi.org/10.1146/annurev.clinpsy.3.022806.091424.
- Leadley K, Clark CL, Caetano R. Couples' drinking patterns, intimate partner violence, and alcohol-related partnership problems. J Subst Abuse. 2000;11(3):253-263. https://doi.org/10.1016/S0899-3289(00)00025-0.
- Leonard KE, Quigley BM. Thirty years of research show alcohol to be a cause of intimate partner violence: Future research needs to identify who to treat and how to treat them. Drug Alcohol Rev. 2017;36(1):7-9. https://doi.org/10.1111/dar.12434.
- Goodsmith N, Ijadi-Maghsoodi R, Melendez RM, Dossett EC. Addressing the urgent housing needs of vulnerable women in the era of COVID-19: The Los Angeles County experience. Psychiatr Serv. 2021;72(3):349-352. https://doi.org/10.1176/appi.ps.202000318.
- Liu M, Zhang N, Hu X, et al. Further divided gender gaps in research productivity and collaboration during the COVID-19 pandemic: Evidence from coronavirus-related literature. J Informetr. 2022;16(2):101295. https://doi.org/10.1016/j.joi.2022.101295.
- Cui R, Ding H, Zhu F. Gender inequality in research productivity during the COVID-19 pandemic. Manufacturing & Service Operations Management. 2022;24(2):707-726. https://doi.org/10.1287/msom.2021.0991.
- Carpenter MA, Cotter DA, Berheide C. "I have no time for anything": Differences in faculty research productivity during the COVID-19 pandemic. ADVANCE Journal. 2021;2(3). https://doi.org/10.5399/osu/ADVJRNL.2.3.3.
- Carr RM, Lane-Fall MB, South E, et al. Academic careers and the COVID-19 pandemic: Reversing the tide. Sci Transl Med. 2021;13(584):eabe7189. https://doi.org/10.1126/scitranslmed.abe7189.
- Smith C, Watchorn D. The pandemic is making it harder for researchers but women are hit the hardest. 4 findings from 80 countries. Impact of Social Sciences Blog, 2020. https://blogs.lse.ac.uk/impactofsocialsciences/2020/09/17/the-pandemic-is-making-it-harder-for-researchers-but-women-are-hit-the-hardest-4-findings-from-80-countries/.
- North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Arch Gen Psychiatry. 2011;68(2):173-180. https://doi.org/10.1001/archgenpsychiatry.2010.131.
- Wolfe HL, Biello KB, Reisner SL, Mimiaga MJ, Cahill SR, Hughto JMW. Transgender-related discrimination and substance use, substance use disorder diagnosis and treatment history among transgender adults. Drug Alcohol Depend. 2021;223:108711. https://doi.org/10.1016/j.drugalcdep.2021.108711.
- Huhn AS, Strain EC, Jardot J, et al. Treatment disruption and childcare responsibility as risk factors for drug and alcohol use in persons in treatment for substance use disorders during the COVID-19 crisis. J Addict Med. 2022;16(1):e8-e15. https://doi.org/10.1097/ADM.0000000000000813.
- Gilbert PA, Saathoff E, Russell AM, Brown G. Gender differences in lifetime and current use of online support for recovery from alcohol use disorder. Alcohol Clin Exp Res. 2022;46(6):1073-1083. https://doi.org/10.1111/acer.14827.
- Khan S, Okuda M, Hasin DS, et al. Gender differences in lifetime alcohol dependence: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Clin Exp Res. 2013;37(10):1696-1705. https://doi.org/10.1111/acer.12158.
- Flentje A, Heck NC, Sorensen JL. Characteristics of transgender individuals entering substance abuse treatment. Addict Behav. 2014;39(5):969-975. https://doi.org/10.1016/j.addbeh.2014.01.011.
- Gonzàlez Castro F, Garfinkle J. Critical issues in the development of culturally relevant substance abuse treatments for specific minority groups. Alcohol Clin Exp Res. 2003;27(8):1381-1388. https://doi.org/10.1097/01.ALC.0000080207.99057.03.
- Mericle AA, de Guzman R, Hemberg J, Yette E, Drabble L, Trocki K. Delivering LGBT-sensitive substance use treatment to sexual minority women. J Gay Lesbian Soc Serv. 2018;30(4):393-408. https://doi.org/10.1080/10538720.2018.1512435.
- Pinedo M, Zemore S, Beltrán-Girón J, Gilbert P, Castro Y. Women's barriers to specialty substance abuse treatment: A qualitative exploration of racial/ethnic differences. J Immigr Minor Health. 2020;22(4):653-660. https://doi.org/10.1007/s10903-019-00933-2.
- Resnicow K, Soler R, Braithwaite RL, Ahluwalia JS, Butler J. Cultural sensitivity in substance use prevention. J Community Psychol. 2000;28(3):271-290. https://doi.org/10.1002/(SICI)1520-6629(200005)28:3<271::AID-JCOP4>3.0.CO;2-I.
- Witherspoon KM, Richardson AW. Sisters in Support Together Against Substances (SISTAS): An alcohol abuse prevention group for Black women. J Ethn Subst Abuse. 2006;5(3):49-60. https://doi.org/10.1300/J233v05n03_03.
- Doornbos MM, Zandee GL, DeGroot J, De Maagd-Rodriguez M. Using community-based participatory research to explore social determinants of women's mental health and barriers to help-seeking in three urban, ethnically diverse, impoverished, and underserved communities. Arch Psychiatr Nurs. 2013;27(6):278-284. https://doi.org/10.1016/j.apnu.2013.09.001.
- Bowleg L. Evolving intersectionality within public health: From analysis to action. Am J Public Health. 2021;111(1):88-90. https://doi.org/10.2105/AJPH.2020.306031.
- Bowleg L, Huang J, Brooks K, Black A, Burkholder G. Triple jeopardy and beyond: Multiple minority stress and resilience among Black lesbians. J Lesbian Stud. 2003;7(4):87-108. https://doi.org/10.1300/J155v07n04_06.
- Crenshaw K. Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review. 1991;43(6):1241-1299. https://doi.org/10.2307/1229039.
- Cerezo A, O'Shaughnessy T. Psychological distress, alcohol misuse and stigma to seek psychological help in a community sample of sexual diverse women of color. Journal of LGBTQ Issues in Counseling. 2021;15(1):59-76. https://doi.org/10.1080/15538605.2021.1868374.
- Carr D. Opinion: Mental health is political. New York Times. September 20, 2022. https://www.nytimes.com/2022/09/20/opinion/us-mental-health-politics.html?smid=nytcore-ios-share&referringSource=articleShare.
- Veldhuis CB, Stuart E, Fallin MD. Five urgent public health policies to combat the mental health effects of COVID-19. Health Affairs Blog. January 27, 2021. https://www.healthaffairs.org/do/10.1377/hblog20210122.959001/full/.
- Fergus S, Zimmerman MA. Adolescent resilience: A framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26(1):399-419. https://doi.org/10.1146/annurev.publhealth.26.021304.144357.
- Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367(9509):528-529. https://doi.org/10.1016/S0140-6736(06)68184-1.
- Opara I, Malik S, Lardier DT, Jr., et al. Alcohol use cravings as a mediator between associated risk factors on increased alcohol use among youth adults in New York during the COVID-19 pandemic. Alcohol Treat Q. 2021;39(4):415-429. https://doi.org/10.1080/07347324.2021.1950091.
- Anderson P, Chisholm D, Fuhr DC. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet. 2009;373(9682):2234-2246. https://doi.org/10.1016/S0140-6736(09)60744-3.
- National Institute on Alcohol Abuse and Alcoholism. State Alcohol-Related Laws During the COVID-19 Emergency for On-Premises and Off-Premises Establishments as of January 1, 2022. Alcohol Policy Information System (APIS). 2022. https://alcoholpolicy.niaaa.nih.gov/sites/default/files/file-page/digest_state_alcohol_policies_in_response_to_covid-19_220101.pdf.
- Miller WR, Tonigan JS, Longabaugh R. The drinker inventory of consequences (DrInC). An instrument for assessing adverse consequences of alcohol abuse. Test manual. 1995.
- Grasso DJ, Briggs-Gowan MJ, Ford JD, Carter AS. Epidemic – Pandemic Impacts Inventory (EPII). Published online 2020.
- Collins LM, Graham JW, Hansen WB, Johnson CA. Agreement between retrospective accounts of substance use and earlier reported substance use. Appl Psychol Meas. 1985;9(3):301-309. https://doi.org/10.1177/014662168500900308.
- Blanchard KA, Morgenstern J, Morgan TJ, Lobouvie EW, Bux DA. Assessing consequences of substance use: Psychometric properties of the Inventory of Drug Use Consequences. Psychol Addict Behav. 2003;17(4):328-331. https://doi.org/10.1037/0893-164X.17.4.328.
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychol Assess. 1994;6(2):117-128. https://doi.org/10.1037/1040-3590.6.2.117.
- WHO ASSIST Working Group. The Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST): Development, reliability, and feasibility. Addiction. 2002;97(9):1183-1194. https://doi.org/10.1046/j.1360-0443.2002.00185.x.
- Bachman JG, Johnston LD, O'Malley PM. Monitoring the Future Questionnaire Responses from the Nation's High School Seniors. Institute for Social Research, University of Michigan; 2012. https://monitoringthefuture.org/results/.
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcohol Clin Exp Res. 2005;29(7):1180-1189. https://doi.org/10.1097/01.ALC.0000171940.95813.A5.
Appendices
These appendices are also available as part of the downloadable PDF: ARCR-43-1-Article05-Keyes.pdf (2.78 MB)
Appendix 1. Description of Studies Included in This Review (N = 51): Sample Sizes, Recruitment Methods, Study Design, and Timing of Start and Stop of Data Collection*| # | First Author | Year | N | Sample Sizes of Subgroups | Sample | Recruitment | Study Design | Data Collection† |
|---|
| Start | End |
|---|
| Prevalence: Single and Repeated Cross-Sectional Studies of General Population Adults |
| 1 | Chandran79 | 2021 | 107,930 | 57% cisgender women | EHR data; no age restrictions | Electronic health records | More than one cross-sectional time point | Pre-pandemic | Early pandemic |
| 2 | Acharya84 | 2022 | 18,808 | 54% cisgender women | Adults | Consumer data | More than one cross-sectional time point | Pre-pandemic | Late 2020 |
| 3 | Beiter85 | 2022 | 102 | 48% cisgender women | Adult health care workers | Convenience | Cross-sectional | Early pandemic | Early pandemic |
| 4 | Boschuetz86 | 2020 | 417 | 84% cisgender women | Adults | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
| 5 | Capasso87 | 2021 | 5,850 | 53% cisgender women | Adult social media users in U.S. | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
| 6 | Grossman88 | 2020 | 832 | 84% cisgender women | Adults | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
| 7 | Kerr89 | 2022 | 1,819 | 52% cisgender women | Adults | Nationally representative | More than one cross-sectional time point | Pre-pandemic | Early 2021 |
| 8 | Knell90 | 2020 | 1,809 | 67% cisgender women | Adults living in U.S. | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
| 9 | Walia91 | 2021 | 3,865 | 50% cisgender women | Health Information National Trends Survey | Nationally representative | Cross-sectional | Early pandemic | Late 2020 |
| Prevalence: Longitudinal/Prospective Studies of General Population Adults |
| 1 | Chartier92 | 2021 | 5,874 | 51% cisgender women | Adults | Nationally representative | Prospective | Early pandemic | Early pandemic |
| 2 | French93 | 2022 | 2,040 | 58% of sample at both time points were cisgender women | Adults living in U.S. | Convenience: Online/social media | Prospective | Early pandemic | Early pandemic |
| 3 | Lannoy94 | 2022 | 86 | 47% cisgender women | People who are HIV+, people with AUD, people with both, and controls with neither | Clinical sample recruited from longitudinal study | Prospective | Early pandemic | Early 2021 |
| 4 | Leventhal95 | 2022 | 8,130 | 52% cisgender women | Adults | Nationally representative | Prospective | Early pandemic | Early 2021 |
| 5 | Meanley96 | 2022 | 2,121 | 58% cisgender women | Participants from two prospective observational cohort studies | Pulled from MACS and WIHS cohorts | Prospective | Pre-pandemic | Late 2020 |
| 6 | Nordeck97 | 2021 | 4,298 | 49% cisgender women | Adults | Nationally representative | Prospective | Early pandemic | Late 2020 |
| 7 | Osaghae98 | 2021 | 267 | 72% cisgender women | Outpatient primary care clinic patients who had received a COVID-19 test | Clinic sample | Prospective | Early pandemic | Early pandemic |
| 8 | Pollard99 | 2020 | 1,540 | 57% cisgender women | Adults | Nationally representative | Prospective | Pre-pandemic | Early pandemic |
| 9 | Tucker100 | 2022 | 1,118 | 52% cisgender women | Participants from RAND ALP study had to report past-year alcohol use. | Nationally representative | Prospective | Pre-pandemic | Early 2021 |
| Specific Populations and Demographic Differences: Adolescents, Young Adults, and Older Adults |
| 1 | Coakley101 | 2021 | 777 | 62% women; 4% non-cisgender; 31% non-heterosexual | College students | Convenience sample of undergraduates | Cross-sectional | Late 2020 | Late 2020 |
| 2 | Hill102 | 2022 | 501 | 71% cisgender women; 0.6% nonbinary or transgender | College students living in U.S. | Undergraduate research pool | Cross-sectional | Late 2020 | Early 2021 |
| 3 | Kim103 | 2022 | Pre-pandemic: 3,643; Pandemic: 4,970 | Pre-pandemic survey: 70% cisgender women, 4% TNB Pandemic survey: 68% cisgender women, 2% TNB | College students | All first- and second-year undergraduates | More than one cross-sectional time point | Pre-pandemic | Early pandemic |
| 4 | Schwartz104 | 2022 | 526 | 74% cisgender women | College students | Convenience: Online/social media | More than one cross-sectional time point | Early pandemic | Late 2020 |
| 5 | Brener105 | 2022 | 7,705 | Not reported | Grades 9–12 | Nationally representative | Cross-sectional | Early pandemic | Late 2021 |
| 6 | Graupensperger106 | 2021 | 572 | 61% cisgender women | Young adults reporting at least one alcoholic beverage in past year | Convenience | Prospective | Pre-pandemic | Early pandemic |
| 7 | Jaffe107 | 2021 | 1,365 | Not reported | College students | Undergraduate research pool | Prospective | Pre-pandemic | Early pandemic |
| 8 | Miech108 | 2021 | 582 | 51% adolescent girls | 12th graders from Monitoring the Future survey | Nationally representative | Prospective | Pre-pandemic | Late 2020 |
| 9 | Romm109 | 2022 | 1,084 | 51% cisgender women; 3% “other” | Young adults | Convenience: Online/social media | Prospective | Pre-pandemic | Late 2020 |
| 10 | Romm110 | 2021 | 1,082 | 51% cisgender women; 3% “other” | Young adults | Convenience: Online/social media | Prospective | Pre-pandemic | Late 2020 |
| 11 | Ryerson111 | 2021 | 302 | 2019 survey: 64% cisgender women 2020 survey: 68% cisgender women | College students | Undergraduates in health classes | Prospective | Pre-pandemic | Early pandemic |
| 12 | Stevenson112 | 2021 | 633 | 43% cisgender women | Young adults | Nationally representative | Prospective/
daily diary | Pre-pandemic | Early pandemic |
| 13 | Eastman113 | 2021 | 6,938 | 54% cisgender women | U.S. adults age 55 and older | Nationally representative | Cross-sectional | Early pandemic | Early pandemic |
| Specific Populations and Demographic Differences: Race/Ethnicity |
| 1 | Hanson114 | 2021 | 62 | 100% cisgender women | American Indian women | Sample from RCT | Prospective | Pre-pandemic | Early pandemic |
| 2 | Hicks115 | 2022 | 323 | 77% cisgender women; 4% TNB participants | Racial/ethnic minority undergraduate students | Convenience: Online/social media | Prospective | Pre-pandemic | Early pandemic |
| Specific Populations and Demographic Differences: Frontline Workers |
| 1 | Beiter85 | 2022 | 102 | 48% cisgender women | Adult health care workers | Convenience | Cross-sectional | Early pandemic | Early pandemic |
| 2 | Hennein119 | 2021 | 1,092 | 72% cisgender women | Health care workers at teaching hospitals | Convenience | Cross-sectional | Early pandemic | Early pandemic |
| Specific Populations and Demographic Differences: Couple Relationships, Pregnancy, and Parenting |
| 1 | Ahlers-Schmit116 | 2020 | 114 | 100% cisgender women | Convenience sample of pregnant women or mothers of infants | Convenience | Cross-sectional | Early pandemic | Early pandemic |
| 2 | McMillan117 | 2021 | 49 | 100% cisgender women | Women age 18 and older who were at least 12 weeks pregnant | Convenience: Online/social media | Cross-sectional | Late 2020 | Late 2020 |
| 3 | Rodriguez118 | 2021 | 118 couples | 50% cisgender women | U.S. adults who consumed at least 12 alcoholic beverages in past year and live with partner | Convenience: Online/social media | Cross-sectional | Late 2020 | Late 2020 |
| Coping, Stress, and Mental Health |
| 1 | Lannoy94 | 2022 | 86 | 47% cisgender women | People who are HIV+, people with AUD, people with both, and controls with neither | Clinical sample recruited from longitudinal study | Prospective | Early pandemic | Early 2021 |
| 2 | Tucker100 | 2022 | 1,118 | 52% cisgender women | Participants from RAND ALP study who had to report past-year alcohol use | Nationally representative | Prospective | Pre-pandemic | Early 2021 |
| 3 | Hennein119 | 2021 | 1,092 | 72% cisgender women | Health care workers at teaching hospitals | Convenience | Cross-sectional | Early pandemic | Early pandemic |
| 4 | Cummings120 | 2021 | 2019: 247;2020: 868 | February 2019: 45% cisgender women; 0% transgender; 2% gender fluid March 2020: 52% cisgender women; 0.3% transgender; 0.6% gender fluid | Adults living in U.S. | Convenience: Online/social media | More than one cross-sectional time point | Pre-pandemic | Early pandemic |
| 5 | Devoto121 | 2022 | 499 | 100% cisgender women | Adult women living in U.S. who agree to share Facebook data | Panel | Cross-sectional | Late 2020 | Late 2020 |
| 6 | Graupensperger122 | 2021 | 1,181 | 60% cisgender women | College students | Convenience | Cross-sectional | Early pandemic | Early pandemic |
| 7 | Helminen123 | 2021 | 68 | 100% cisgender women | Community sample of trauma-exposed adult women | Convenience | Cross-sectional | Early pandemic | Late 2020 |
| 8 | Martinez124 | 2022 | Pre-pandemic: 1,291; Early pandemic: 812 | 61% cisgender women at baseline | Two cross-sectional NAS samples | Nationally representative | More than one cross-sectional time point | Pre-pandemic | Early pandemic |
| 9 | Nesoff125 | 2021 | 2,175 | 85% cisgender women; 4% TNB people | Adults living in U.S. | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
| 10 | Vogel126 | 2021 | 180 | 65% cisgender women | Recruited through Qualtrics | Convenience: Online/social media | Cross-sectional | Early pandemic | Late 2020 |
| Transgender and Nonbinary Populations |
| 1 | Coakley101 | 2021 | 777 | 62% women; 4% non-cisgender; 31% non-heterosexual | College students | Convenience sample of undergraduates | Cross-sectional | Late 2020 | Late 2020 |
| 2 | Hicks115 | 2022 | 323 | 77% cisgender women; 4% TNB participants | Racial/ethnic minority undergraduate students. | Convenience: Online/social media | Prospective | Pre-pandemic | Early pandemic |
| 3 | Dyar127 | 2022 | 429 | 73% cisgender women; 15% nonbinary; 5% genderqueer; 4% nonconforming; 3% "another identity" | Same criteria as Dyar 2021 study | Convenience: Online/social media | Prospective | Late 2020 | Early 2021 |
| 4 | Salerno128 | 2021 | 509 | 78% AFAB: 69% cisgender, 9% transgender 1% nonbinary, 0.9% queer gender | Sexual and gender minority full-time college students | Convenience: Online/social media | Cross-sectional | Early pandemic | Late 2020 |
| 5 | Sumetsky129 | 2022 | 247 | 59% cisgender women, 15% TNB | Adults in Allegheny County, PA | Convenience: Online/social media | Cross-sectional | Early pandemic | Late 2020 |
| 6 | Zhang130 | 2022 | 366 | 47% cisgender women, 4% trans women, 8% trans men, 15% nonbinary, 2% genderqueer, 3% another gender | LGBTQ+ college students | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
| 7 | Akré131 | 2021 | 3,245 | 84.9% cisgender straight; 3.7% cisgender gay or lesbian; 7.0% cisgender bisexual; 3.8% cisgender men who have sex with men and women who have sex with women but do not identify as LGBT; 0.6% transgender | Adults in Atlanta, GA; Chicago, IL; New Orleans, LA; New York, NY; and Los Angeles, CA | Panel | Cross-sectional | Early Pandemic | Late 2020 |
| Sexual Minority Women |
| 1 | Dyar127 | 2022 | 429 | 73% cisgender women; 15% nonbinary; 5% genderqueer; 4% nonconforming; 3% "another identity" | Same criteria as Dyar 2021 study | Convenience: Online/social media | Prospective | Late 2020 | Early 2021 |
| 2 | Salerno128 | 2021 | 509 | 78% AFAB and 69% of sample was cisgender; 9% transgender; 1% nonbinary; 0.9% queer gender | Sexual and gender minority full-time college students | Convenience: Online/social media | Cross-sectional | Early pandemic | Late 2020 |
| 3 | Dyar132 | 2021 | 212 | 74% cisgender women; 18% genderqueer or nonbinary; 9% another gender | Age 18–25; live in U.S.; lesbian, bisexual, pansexual, or queer; AFAB; reported four or more drinks at least twice and/or using cannabis in past month | Convenience: Online/social media | Prospective/EMA/daily diary study | Late 2020 | Early 2021 |
| 4 | Peterson133 | 2021 | 170 | 64% cisgender women | U.S. Adults | Convenience: Online/social media | Cross-sectional | Early pandemic | Early pandemic |
*Articles are listed in the order in which they appear in the manuscript. Some studies are listed in more than one section of the table.
†Time periods for start and stop of research studies: Pre-pandemic (Before March 2020); Early pandemic (March–May 2020); Late 2020 (June–December 2020); Early 2021 (January–May 2021); Late 2021 (June–December 2021).
Note: AFAB, assigned female at birth; AUD, alcohol use disorder; COVID-19, coronavirus disease 2019; EHR, electronic health record; EMA, ecological momentary assessment; HIV+, human immunodeficiency virus–positive; LGBT, lesbian, gay, bisexual, transgender; LGBTQ+, lesbian, gay, bisexual, transgender, and queer or questioning; MACS, Multicenter AIDS Cohort Study; NAS, National Alcohol Survey; RAND ALP, RAND American Life Panel; RCT, randomized controlled trial; TNB, transgender and nonbinary; WIHS, Women's Interagency HIV Study.
Appendix 2. Description of Studies Included in This Review (N = 51): Measurement of Alcohol Use and Changes in Alcohol Use and Brief Findings*| # | First Author | How was alcohol use measured? | How were changes in alcohol use measured? | Gender Differences |
|---|
| Gender differences? | Findings |
|---|
| Prevalence: Single and Repeated Cross-Sectional Studies of General Population Adults |
| 1 | Chandran79 | SBIRT and intoxication admissions; AUDIT | Pre- and post/during pandemic data | Yes | Weekly SBIRT screens similar across gender in the pre-pandemic wave, then increased more for cisgender women than cisgender men. |
| 2 | Acharya84 | Bi-weekly alcohol expenditures | Pre- and post/during pandemic data | No | Both cisgender men and women had decreased in spending on alcohol during pandemic, gender differences in spending during pandemic were not significant. |
| 3 | Beiter85 | AUDIT | Retrospective recall of pre-pandemic AUDIT | Yes | Cisgender men higher AUDIT than cisgender women; all reported increases in AUDIT compared with pre-pandemic; no gender by time interaction assessed. |
| 4 | Boschuetz86 | AUDIT-C, quantity and frequency, binge drinking | Retrospective report of current drinking in past vs. drinking now | Yes | Cisgender women reported more AUDIT-C symptoms after start of pandemic, cisgender men did not; no changes in alcohol frequency. |
| 5 | Capasso87 | Self-perceptions of change in alcohol use | Self-perceived changes in alcohol use | Yes | Among those who reported increased drinking, 61% were cisgender women compared to 39% who were cisgender men (statistically significant). Younger participants more likely to report increased drinking, but no interactions examined between age and gender. |
| 6 | Grossman88 | Days consumed, drinks consumed, binge drinking | N/A | No | No gender differences in number of days consumed alcohol, total drinks, or binge drinking. |
| 7 | Kerr89 | Graduated frequency series. DSM-V AUD criteria | Pre- and post/during pandemic data | Yes | Daily drinking increased for both cisgender men and women, as did AUD mild and moderate/severe; moderate/severe AUD increased more for cisgender women than for men; volume, especially wine and spirit volume, increased more for cisgender women than men. |
| 8 | Knell90 | Ever use and current quantity and frequency from BRFSS | Self-perceived changes in alcohol use | No | No gender differences in self-perceptions of changes in alcohol use since start of pandemic. |
| 9 | Walia91 | Quantity | N/A | Yes | Significant gender differences, but no pairwise differences reported. Cisgender men had double the rates of reporting 13 or more drinks in a week than did cisgender women; other drinking levels did not differ. |
| Prevalence: Longitudinal/Prospective Studies of General Population Adults |
| 1 | Chartier92 | Alcohol use frequency | Self-report of current drinking at more than one time point | Yes | June 2020: cisgender women drank less than cisgender men; in change models, increased drinking during the month was no different between cisgender men and women, but cisgender women less likely to decrease drinking. |
| 2 | French93 | "In the past three months, has alcohol consumption increased, stayed the same, or decreased?" | Self-perceived changes in alcohol use | Yes | Cisgender women significantly less likely than cisgender men to say that alcohol consumption had increased. |
| 3 | Lannoy94 | AUDIT | Pre- and post/during pandemic data | No | No sex differences, stable AUDIT scores between assessments |
| 4 | Leventhal95 | Frequency and intensity of drinking | Self-report of current drinking at more than one time point | Yes | Cisgender women comprised higher percentage of minimal and moderate/late decreasing trajectory group; lower percentage in moderate/early increasing, and near daily/early increasing |
| 5 | Meanley96 | Reported frequency with which they consumed at least five (cisgender women) or six (cisgender men) alcoholic beverages in one sitting. | Pre- and post/during pandemic data | Yes | Cisgender men significantly more likely to be in the ‘any binge drinking’ trajectory group. Significant gender by time interaction; both cisgender men and women exhibited significant binge drinking decreases at time three compared to time one; decrease larger in cisgender men. |
| 6 | Nordeck97 | Number of drinking days per week | Self-report of current drinking at more than one time point | Yes | Cisgender women had lower number of drinking days overall; both cisgender women and men increased drinking days; cisgender men increased more. |
| 7 | Osaghae98 | AUDIT-C | Self-report of current drinking at more than one time point | Yes | 36.1% of cisgender women and 32.9% of cisgender men reported hazardous drinking at baseline. Did not test gender by time interaction. |
| 8 | Pollard99 | Days drank, number of drinks, heavy drinking days | Self-report of current drinking at more than one time point | Yes | Days consumed increased more for cisgender women; number of drinks increased more for cisgender men; heavy drinking days increased more for cisgender women; SIP scale not different |
| 9 | Tucker100 | Quantity and frequency; Alcohol problems assessed with the Short Inventory of Problems195 | Pre- and post/during pandemic data | Yes | Analyses were stratified by gender. Cisgender men's alcohol use started out higher than cisgender women but declined whereas cisgender women's stayed static. By time 3, drinking levels were about the same. Both cisgender men and cisgender women had increased alcohol problems over time. Coping and social reasons for drinking and loneliness had distinct associations with alcohol use, alcohol problems, and change over time and these varied by gender. |
| Specific Populations and Demographic Differences: Adolescents, Young Adults, Older Adults |
| 1 | Coakley101 | Quantity and frequency | Self-report of current drinking at more than one time point | Yes | Pre-pandemic (retrospectively reported), cisgender men drank more than cisgender women who drank more than TNB participants; during pandemic, consumption increased across groups, but remained cisgender men > cisgender women > TNB; cisgender men and TNB participants had greatest percent change during pandemic. |
| 2 | Hill102 | AUDIT | N/A | Yes | Cisgender men had higher AUD symptoms than cisgender women. No pre-pandemic data and no time by gender interaction tested. |
| 3 | Kim103 | AUDIT | N/A | Yes | Increases in AUD more concentrated among cisgender women |
| 4 | Schwartz104 | "During the last two months, how often have you engaged in alcohol use?" | Retrospective report of current drinking in past vs drinking now | No | Gender differences tested but not significant. Alcohol use worsened between spring and fall 2020. |
| 5 | Brener105 | Quantity and frequency, current binge drinking | Self-perceived changes in alcohol use | Yes | Cisgender women higher than cisgender men for current and binge drinking; no differences in perceived changes since pandemic. Sexual minority students reported higher current alcohol use, binge drinking, and drinking during the pandemic than did heterosexual students. |
| 6 | Graupensperger106 | Quantity/frequency; Drinks per occasion | Self-report of current drinking at more than one time point | Yes | At baseline, cisgender women lower drinking than cisgender men; drinking declined at follow-up; declines were greater for cisgender men than cisgender women (significant interaction). |
| 7 | Jaffe107 | Quantity and frequency | Self-report of current drinking at more than one time point | Yes | Cisgender men greater drinking days, greater drinks per day (both across years and within 2020); college students did not increase drinking in spring 2020 as was typical in previous years; no gender by time interaction reported. |
| 8 | Miech108 | "Think back over the last 2 weeks. How many times have you had five or more drinks in a row?" | Pre- and post/during pandemic data | No | Study found that past 2-week binge declined from spring to summer 2020 overall; no overall gender differences; did not test time by gender interaction. |
| 9 | Romm109 | Past 30-day quantity and frequency | Self-report of current drinking at more than one time point | Yes | Baseline drinking was lower for cisgender men than cisgender women; increases in alcohol use during pandemic greater for cisgender men than cisgender women |
| 10 | Romm110 | "Compared to before COVID-19, are you doing more or less of the following: drinking alcohol?" | Self-perceived changes in alcohol use | No | 41.3% of participants reported increased alcohol use; no gender difference in self-reported increased alcohol use |
| 11 | Ryerson111 | Typical total weekly volume of alcohol consumption | Self-report of current drinking at more than one time point | No | No gender differences in alcohol consumption; 2020 cohort decreased alcohol consumption compared with 2019 cohort, especially those > 21; gender interaction with time was statistically significant, but direction not reported. |
| 12 | Stevenson112 | Any drinking; drinking intensity on drinking days | Self-report of current drinking at more than one time point | Yes | Cisgender men more likely to report any drinking; no change in drinking during COVID; no gender interaction reported. |
| 13 | Eastman113 | "Over the past week, have any of your usual daily activities or behaviors changed?" | Self-perceived changes in alcohol use | Yes | Of those who said they were drinking more than usual, 58.9% were cisgender women. |
| Specific Populations and Demographic Differences: Demographic Differences by Race/Ethnicity |
| 1 | Hanson114 | Quantity/frequency | Retrospective report of current drinking in past vs. drinking now | N/A | 24.2% of cisgender women reported drinking more now and 50% reported binge drinking since pandemic started; 54.8% had 8+ drinks per week. |
| 2 | Hicks115 | Alcohol use frequency from AUDIT | Pre- and post/during pandemic data | Yes | No differences by sexual identity; cisgender men more likely to decrease alcohol use during pandemic compared to cisgender women. No significant gender differences between cisgender and TNB participants. |
| Specific Populations and Demographic Differences: Frontline Workers |
| 1 | Beiter85 | AUDIT | Retrospective recall of pre-pandemic AUDIT | Yes | Cisgender men higher AUDIT than cisgender women; all reported increases in AUDIT compared with pre-pandemic; no gender by time interaction assessed. |
| 2 | Hennein119 | AUDIT-C | N/A | No | Cisgender women were no more likely than men to report AUD symptoms despite higher rates of PTSD. |
| Specific Populations and Demographic Differences: Couple Relationships, Pregnancy, and Parenting |
| 1 | Ahlers-Schmit116 | Unclear measurement | Self-perceived changes in alcohol use | N/A | Increases in alcohol use significantly higher postpartum than during pregnancy. |
| 2 | McMillan117 | Epidemic Pandemic Impact Inventory (EPII)196 | Self-perceived changes in alcohol use | N/A | Almost one-third (28%) reported that they or their partner's alcohol consumption had increased since the start of the pandemic. |
| 3 | Rodriguez118 | Daily Drinking Questionnaire;197 Shortened Inventory of Problems-Alcohol and Drugs scale;198 Drinking to cope using two visual analog scales | N/A | Yes | Cisgender men reported significantly more alcohol-related problems than did cisgender women, but drinking levels did not differ by gender. Cisgender women's drinking was significantly associated with their partner's drinking and stress; cisgender men's drinking was unrelated to their partner's drinking or stress. Cisgender women's levels of stress were unrelated to their drinking. |
| Coping, Stress, and Mental Health |
| 1 | Lannoy94 | AUDIT | Pre- and post/during pandemic data | No | No sex differences, stable AUDIT scores between assessments |
| 2 | Tucker100 | Quantity and frequency; Alcohol problems assessed with the Short Inventory of Problems195 | Pre- and post/during pandemic data | Yes | Analyses were stratified by gender. Cisgender men's alcohol use started out higher than cisgender women but declined whereas cisgender women's stayed static. By time 3, drinking levels were about the same. Both cisgender men and cisgender women had increased alcohol problems over time. Coping and social reasons for drinking and loneliness had distinct associations with alcohol use, alcohol problems, and change over time and these varied by gender. |
| 3 | Hennein119 | AUDIT-C | N/A | No | Cisgender women were no more likely than cisgender men to report AUD symptoms, despite higher rates of PTSD. |
| 4 | Cummings120 | Quantity, frequency, and two items adapted from Drinking Motives Questionnaire199 | Pre- and post/during pandemic data | Yes | No differences in drinking to cope comparing pre- and during pandemic samples (did not look at gender differences). Significant associations between COVID-19 stress and drinking to cope for cisgender men and women but associations were stronger for men. |
| 5 | Devoto121 | AUDIT-C; Alcohol, Smoking, and Substance Involvement Screening Test200 | N/A | N/A | Among cisgender women, high-risk alcohol associated with significantly higher levels of depression and anxiety than lower risk use. Cisgender women with moderate drinking risks reported higher levels of social support than cisgender women with high-risk drinking. Almost 17% said that they increased their drug or alcohol use to cope with relationship problems. |
| 6 | Graupensperger122 | Daily Drinking Questionnaire,197 binge drinking item from Monitoring the Future questionnaire201 | N/A | No | No gender differences in rates of binge drinking or number of drinks per week. |
| 7 | Helminen123 | AUDIT-C | N/A | N/A | Nearly half (47.1%) of the sample reported alcohol use consistent with probable AUD. |
| 8 | Martinez124 | Two drinking to cope questions adapted from the Drinking Motives Questionnaire199 | Pre- and post/during pandemic data | Yes | Among cisgender women, 13.8% reported drinking to cope prior to the pandemic and 15.6% reported drinking to cope during the pandemic, compared to 10.7% before and 17% during the pandemic for cisgender men. These rates were not statistically different. Among cisgender women, those with moderate to severe symptoms of depression or mild symptoms of anxiety were significantly more likely to report drinking to cope. No significant associations were identified for cisgender men. |
| 9 | Nesoff125 | Adapted quantity and frequency items from NSDUH | Self-perceived changes in alcohol use | Yes | Odds of high-risk drinking were significantly elevated for cisgender women when controlling for stress, depressive symptoms, and household job loss. Cisgender men had lower odds of high-risk drinking than cisgender women. |
| 10 | Vogel126 | Short Inventory of Problems—Alcohol and Drugs (SIP-AD)198 | N/A | No | Sex, race/ethnicity, marital status, and other pandemic-related variables were not associated with SIP-AD scores. |
| Transgender and Nonbinary Populations |
| 1 | Coakley101 | Quantity and frequency | Self-report of current drinking at more than one time point | Yes | Pre-pandemic (retrospectively reported), cisgender men drank more than cisgender women who drank more than TNB people. During pandemic, consumption increased across groups, but cisgender men still drank more than cisgender women, who drank more than TNB people. Cisgender men and TNB people had greatest percentage change during pandemic. |
| 2 | Hicks115 | Alcohol use frequency from AUDIT | Pre- and post/during pandemic data | Yes | No differences by sexual identity; cisgender men were more likely than cisgender women to decrease alcohol use during pandemic. No significant gender differences between cisgender and TNB participants. |
| 3 | Dyar127 | Daily drinking questionnaire,197 quantity | Self-report of current drinking at more than one time point | No | No significant differences between cisgender women and TNB participants for alcohol use or drinking to cope. |
| 4 | Salerno128 | Indicated if alcohol use had changed since the start of pandemic. | Self-perceived changes in alcohol use | Yes | The effect of increased alcohol use on psychological distress since the start of COVID-19 was nonsignificant for AMAB but was significant for AFAB people. |
| 5 | Sumetsky129 | Quantity and frequency of drinking and number of days of intoxication | Retrospective report of past drinking vs. current drinking | Yes | Compared to cisgender women, cisgender men had more drinks on drinking days during pandemic, and more days intoxicated pre-pandemic. There were no significant differences for TNB people. |
| 6 | Zhang130 | AUDIT | Self-perceived changes in alcohol use | Yes | Transgender and GNC people had lower problem drinking, and were less likely to have perceived increase in their drinking during COVID-19 than cisgender participants. |
| 7 | Akré131 | PROMIS Alcohol Use Negative Consequences 7-item short-form scale | Self-report of changes in alcohol consumption due to the pandemic | Yes | No substantial difference in rates of increased alcohol use between transgender and cisgender, straight respondents, but some elevated use among cisgender, sexual minority respondents. |
| Sexual Minority Women |
| 1 | Dyar127 | Daily drinking questionnaire,197 quantity | Self-report of current drinking at more than one time point | No | No significant differences between cisgender women and TNB participants for alcohol use or drinking to cope. |
| 2 | Salerno128 | Indicated if alcohol use had changed since the start of pandemic. | Self-perceived changes in alcohol use | Yes | The effect of increased alcohol use on psychological distress since the start of COVID-19 was non-significant for AMAB but significant for AFAB people. |
| 3 | Dyar132 | AUDIT, Drinking motives, Brief Young Adult Alcohol Consequences Questionnaire202 | Self-perceived changes in alcohol use | N/A | Nearly all participants reported more anxiety and depression in the past month compared to before the pandemic; approximately half also reported increases in alcohol and cannabis use. |
| 4 | Peterson133 | AUDIT | Self-perceived changes in alcohol use | Yes | SMW more likely to report alcohol use increased since beginning of pandemic than SMM and cisgender heterosexual women |
*Within each section, studies are listed in the order in which they are cited. Some studies are listed in more than one section.
Note: AFAB, assigned female at birth; AMAB, assigned male at birth; AUD, alcohol use disorder; AUDIT, Alcohol Use Disorders Identification Test; AUDIT-C, Alcohol Use Disorders Identification Test-Consumption; BRFSS, Behavioral Risk Factor Surveillance System; COVID-19, coronavirus disease 2019; DSM-V,Diagnostic and Statistical Manual of Mental Disorders, fifth edition; GNC, gender nonconforming; N/A, not applicable (in the Gender Differences column, N/A indicates that the sample includes cisgender women only); NSDUH, National Survey on Drug Use and Health; PROMIS, Patient-Reported Outcomes Measurement Information System; PTSD, post-traumatic stress disorder; SBIRT, screening, brief intervention, and referral to treatment; SIP-AD, Short Inventory of Problems–Alcohol and Drugs; SMM, sexual minority men; SMW, sexual minority women; TNB, transgender and nonbinary.